Congratulations to all the winners of tutors prizes at the 2024 Annual Teachers Conference. Below you can read feedback from students placed with each of the winners:
Teaching Excellence Award: Dr Yulia Peysakhova, Cavendish Health Centre
“My supervisor Dr Peysakhova is so awesome. She actually wants us to learn and gives us opportunity to do this.”
“Dr Peysakhova doesn’t waste time. She makes sure everything is a learning opportunity and she’s so well versed in teaching younger years. Very lucky to be put on this placement. Thank you!”
“She’s so awesome. Would definitely recommend her to be put forward to teach more students.”
“She lets us take calls to practice history taking. Her advice is actually targeted and useful. I’ve learnt so much from her.”
Teaching Excellence Award: Dr Sabri Trepca, Barlby Surgery
“Dr Trepca is very encouraging and teaches useful and relevant lessons during his clinic.”
“Dr Sabri Trepca was an excellent teacher who discussed all the cases that presented with us – he was kind and understanding and gave good advice – contributing to our clinical knowledge and general life knowledge. Dr Sabri created a relaxed environment for us – where we felt comfortable to speak up and ask questions. He was non-judgmental and did not use harsh language. He showed us how to deal with difficult patients, how to perform and interpret findings from otoscopy/ophthalmoscopy/blood pressure measurements/urine dipsticks/blood results, what to notice in a patient when they walk in – signs that show a child is ill – what to do when in clinical doubt. He covered a vast scope of topics with us including multiple myeloma, nutrient deficiencies, ear infections, tonsillitis, vitamin deficiencies, 8 week checks, smear tests etc It was a pleasure to be on placement with him – he worked hard and made it as enjoyable and as engaging as he could.”
Teaching Excellence Award: Dr Stephanie Hughes, The Friarsgate Practice
“Dr Hughes was absolutely amazing, such a well organised and useful placement This was genuinely one of my favourite placements of medical school. I was going to GP not expecting to enjoy it much as I had not enjoyed it in previous years due to insufficient opportunity to get involved with the team. However I had the opportunity to get involved with multiple members of the MDT, run numerous clinics and decide patient plans. I also think this placement prepared me for being a doctor – I got practice writing patient prescriptions, writing referral letters, requesting investigations and I was well supported by all the doctors who supervised me. I would really strongly recommend this placement. All the doctors were instrumental in my education especially Dr Stephanie Hughes who is an excellent GP tutor.”
Supporting the Student Experience Practice Award: KS Medical Centre, Southall
“KS Medical Centre welcomed us so well and made us feel a part of the team. Dr Kamini was an amazing mentor and teacher, who always went above and beyond to give us useful teaching and experience. She was very passionate about us getting more confident throughout the 8 weeks and she ensured that we became more confident with our own skills and knowledge. Both Dr Kamini and Dr Ross taught us really well and also understood the importance of getting our sign offs done so we felt really comfortable and did not have to worry about not getting things done.”
“Overall, they were incredible and definitely should be praised for giving both me and my partner such an enjoyable time during MICA. Dr Kamini Gautam+ Dr Ross Mcjannette were incredibly accomodating. They went above and beyond in support, teaching and general care. I have never enjoyed and learnt so much from a placement before.”
Supporting the Student Experience Practice Award: Millbank Medical Centre, Westminster
“This was the best medical placement I have had up to date in my medical education. The structure and organisation from the get go with regards to teaching and the forms we needed, the additional opportunities provided by Dr McLaughlin; the hospice, the district nurses and the coroners court. She went above and beyond what is required for our medical teaching and provided experiences that I will not forget throughout my professional career. All the GPs, in particular Dr Dee and Dr Patel, made sure to have us as included as possible within the team and would actively involve us in any learning experiences available. The teaching was centred on what we wanted to get out of the placement and made us feel involved with the practice team as well as being able to take control of our learning was something I haven’t experienced at any other placement. I have no improvements to recommend. This experience was incredible. If there are any accolades awarded I would like to nominate both the practice and Dr Niamh McLaughlin as it is well deserved for the effort and care they put in their teaching. Truly exceptional. Again just to emphasise any medical student should feel privileged to have the opportunity to learn at Millbank! Absolutely fantastic GP tutor and team at the practice, really welcoming, keen to learn and to teach and open to answering any questions. Niamh McLaughlin is a great mentor, who is keen to facilitate our learning and catered our timetable to what we wanted to achieve. Couldn’t have been better.”
Supporting the Student Experience Award: The Croft Medical Centre, Leicester
“The entire team at the croft medical center was so lovely! I had the best time, all of the reception staff, all nurses and of course all of the lovely GP’s I got to spend time with were all kind beyond end. A HUGE thank you to Dr Makda for being such a great student mentor, his team gave me a perfect amount of authority during the time I was there; I was allowed my own clinics but was guided in terms of management and quieres along the way. He was an outstanding GP and even more so teacher; very understanding, very enthusiastic and extremely kind. I can only recommend this practice highly. Generally as a GP service, this practice was by far one of the most organised and thought through practices I have ever seen. From splitting the workload to timetabling students, whether these were from London universities or Leicester university, all of it was done seamlessly with absolutely no problems; no IT problems, no reasons to be shy, no problems accessing the GP center. It was top tier.”
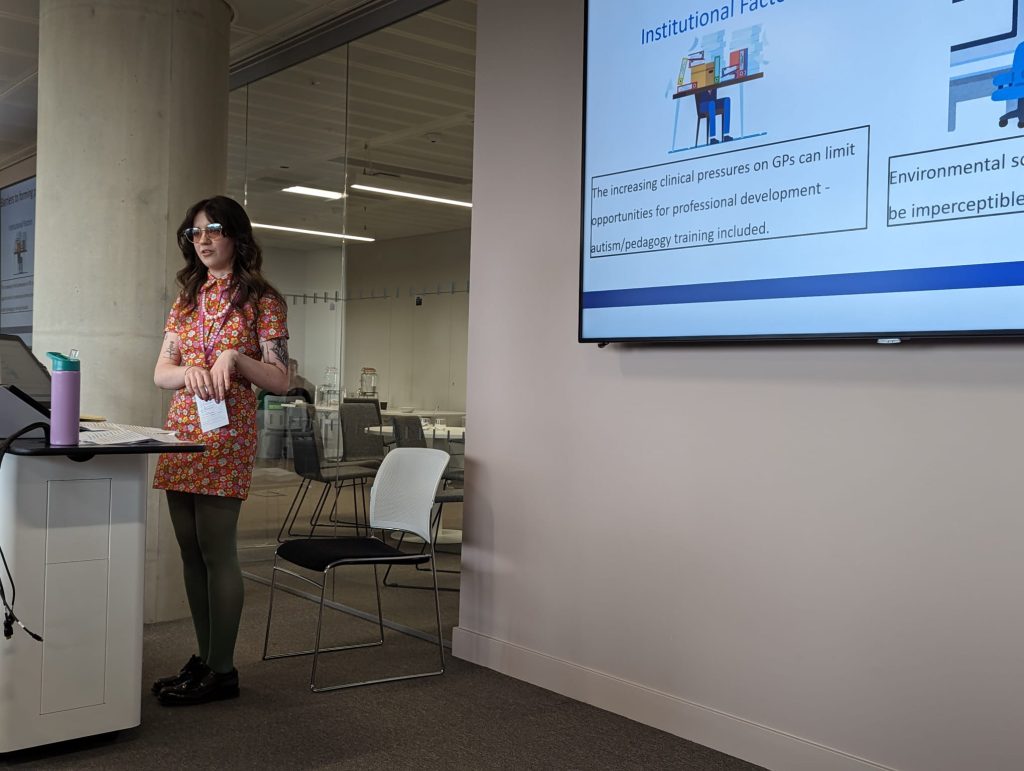
Outstanding contribution to teaching: Fulham Medical Centre
Jan 2024: “The entire team at the Fulham Medical Centre was exceptional. In particular, Dr Libby Pearson and Dr George Hawche went above and beyond in their teaching and support, making this one of the most enjoyable and useful placement I have had to date.”
Oct 2023: “All of the members of the team at this GP were extremely friendly and welcoming and made us feel at home in the practice. In particular Dr Tim and Dr Libby gave us excellent teaching and feedback. They always picked out specific patients for us to see which would be most useful to our learning, which I found very beneficial.”
Sept 2023: “The entire team were very kind and inviting. They all welcomed us and would ensure that any queries we had were dealt with efficiently. Moreover, the doctors were very kind. Particularly, the leads (Libby Pearson and Tim McNicholas) always ensured we were seeing interesting patients and were fulfilling any goals or objects we had set out. Dr Pearson is a very wonderful mentor and I understand why she has won so many teaching awards! She had a very kind and reassuring demeanour. If any issues had arisen, I would have felt more than happy to discuss with her.”
August 2023: “Dr Libby Pearson, Dr Tim Mcnicolas and Dr George Hawche were excellent in providing opportunities for me to clerk patients independently, while feeling involved in the team”
“This GP practice is a shining beacon of what a GP team can achieve. Dr Pearson, Dr Hawche and Dr Tim (forgetting his last name) were all thorough and patient teachers despite having busy schedules. All staff members at the practice were warm and welcoming and provided any support needed.”
Oct 2022: “Dr Pearson was incredibly supportive throughout the placement. Along with support from Dr MacNicholas, the practice was very welcoming and granted me a high level of autonomy and independence which was very helpful for my professional development.”
July/Aug 2022: “The team at Fulham Medical Centre were amazing! I felt so welcomed by all the doctors and staff there. Dr Pearson was so lovely and eager to teach, and gave us our own clinic from week 1 so we could practice independent interactions with patients. Dr George was also particularly enthusiastic about teaching us regarding various topics and cases presented.”
“This was such a great placement, my anxieties of continuing clinical years after finishing my BSc were mostly gone after this placement! My confidence greatly increased due to the guidance provided by the team here.”
Read Annual Teachers Conference 2024: Tutor prizes in full
 by Dr Sarah Green
by Dr Sarah Green



 As part of its commitment to promoting conversations between students studying healthcare across the globe, MEdIC have created a Global Creative Competition. Initially established in 2020, the competition invited students to understand and reflect on the global COVID-19 pandemic. Further iterations of the competition have focussed on the themes of: Global Unity (2022) and the United Nations Sustainability goals (2024) reflecting international priorities. In 2024 the competition was also opened to all healthcare profession students from across the globe to reflect the multidisciplinary nature of healthcare delivery globally.
As part of its commitment to promoting conversations between students studying healthcare across the globe, MEdIC have created a Global Creative Competition. Initially established in 2020, the competition invited students to understand and reflect on the global COVID-19 pandemic. Further iterations of the competition have focussed on the themes of: Global Unity (2022) and the United Nations Sustainability goals (2024) reflecting international priorities. In 2024 the competition was also opened to all healthcare profession students from across the globe to reflect the multidisciplinary nature of healthcare delivery globally.