 by Dr Sarah Green
by Dr Sarah Green
Dr Catherine Ramsay is a GP in west London and has been teaching Imperial medical students for many years. We caught up with her to find out how she makes every teaching moment count.
In a busy clinical day, what helps you weave teaching into the normal flow of patient care?
I check regarding the student’s prior experience in primary care and check if they need any particular clinical skills or formative assessments to be completed which enables me to tailor any teaching to the student’s learning needs. I also try to involve them in small active roles like summarising the history or suggesting the management plan and this helps with engagement. I think aloud during consultations, discussing my reasoning as I go along to the patient and ask the student to write down any queries they might have during the consultation. I get them to reflect a learning point after every case on a particular aspect of the consultation depending on the level of the student, for example, addressing ideas, concerns and expectations or the management plan. I also try to mix up teaching techniques, for example running a joint clinic where I might take the history and the student do the management plan and then swapping over roles.
Can you describe any useful student learning activities if you’re tight on time?
I might give the student a specific task like giving lifestyle advice or safety netting the consults, or for them to do a clinical skill such as taking the blood pressure whilst I am typing in the patient record. I might acknowledge that we are running really late and talk about why that might change my consultation style and get the student to pick out any cues or health promotion opportunities I might have missed. With admin I might ask them to type, draft a referral letter or fit note. Another option might be to give them a task of looking through the prescription requests.
What strategies have you found most helpful for having effective feedback conversations with students?
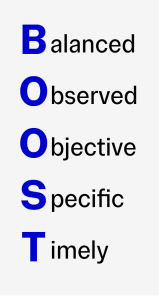
Feedback is most effective when the student has indicated what they feel is the priority for them in their learning, but I do try to use the BOOST model or I tend to break down feedback into the domains used in assessments like clinical skills, consideration of the clinical issues and management plans. I always ask the student to reflect on what they have done well and achieved and finish again on a positive or something they can reflect on. In communicating potential improvements, I like to ask the students what they might do differently on a better day to put a positive light on things.
How do you adapt your teaching approach for learners at different stages of training?
I tend to teach final year students, but I do also teach nursing students in my diabetic clinics. We might have a chat about their confidence levels at the start, and I’ll ask the student to consider what they want to focus on or get feedback about. For less experienced students it might be practising taking a focused history when I might be the patient or working on communication skills such as communicating results. For more experienced learners I tend to let the students run their own clinics, report back with a suggested management plan or perhaps ask them to discuss the clinical issues. I think it’s important to reinforce recognising a sick patient in primary care, for students to recognise their limits and when to ask for support from a senior.
And finally, what’s one small change you’ve made that’s made teaching feel more sustainable or satisfying alongside your service commitments?
I ensure I allow time for students to give feedback as I really appreciate this so that I can continue to adapt and make my teaching relevant. I think it’s important for learning to be fun – I feel it improves everyone’s enthusiasm and enjoyment!