by Dr Jo Harris
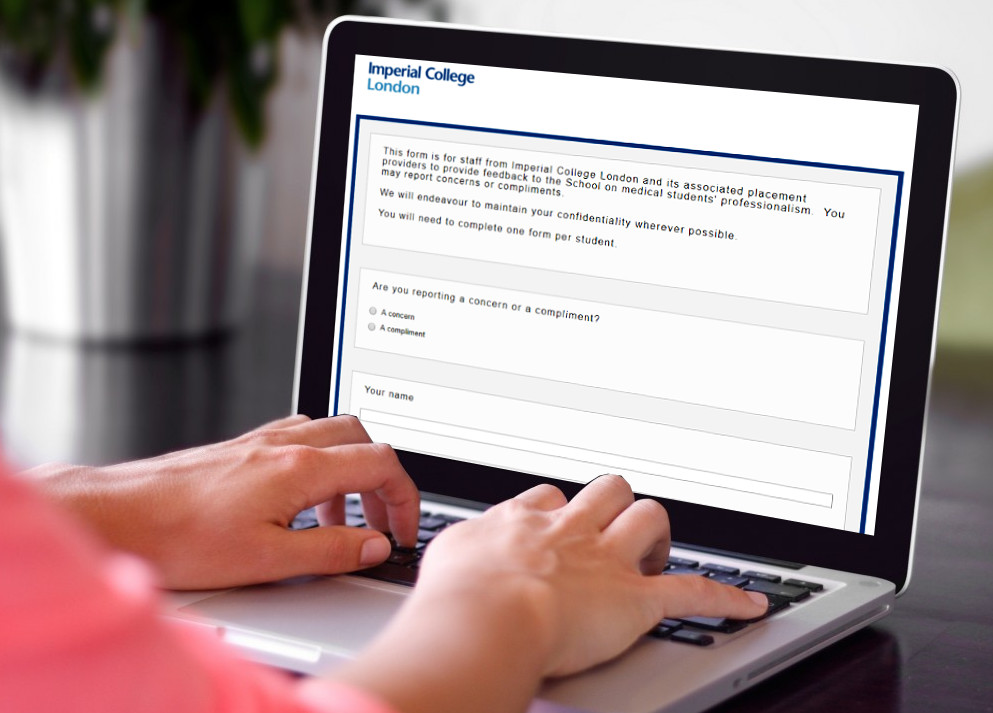
I would like to update our community GPs on the new School of Medicine reporting form. This form known as the ‘concerns and compliments’ form was introduced as an optional addition to the end of year sign-off form, completed after every placement, in the academic year 2017/18. The launch has been successful and it is particularly good to see that our GPs have engaged well with this form.
Overall, we received 68 compliments and 14 concerns across all our sites for the whole School in 17/18. The forms are not meant to be completed for every student, but for those who either impress or who cause concern especially in terms of their professional behaviour.
The range of roles of those who have submitted forms so far is shown in the table below: –
Table 1: Concerns and compliments 2017/18 by role of submitter
| Reported by:- | Compliments | Concerns |
| Faculty | 7 | 0 |
| Consultant | 15 | 3 |
| GP | 14 | 1 |
| Junior doctor | 9 | 0 |
| Teaching fellow | 9 | 9 |
| Nurse | 4 | 0 |
| Teaching coordinator | 10 | 1 |
| TOTAL | 68 | 14 |
Students told us the sign-off form provided little feedback on their achievements or professionalism, especially when they had done something in excess of Imperial expectations. We wanted to ensure that excellence was being recognised and that the students knew there was oversight of their performance even on placements further afield.
Teachers are sometimes unwilling to write negative comments or fail to sign-off students as there is a worry this would affect their progression on the course. This means that low–level concerns – such as attendance issues or timekeeping – can often go unreported, and students could have similar issues in more than one attachment. We are keen to know about these low-level concerns since there is often an underlying welfare issue that can be addressed to support the student before this becomes a major issue. The GMC have also highlighted that Schools should identify cases where student behaviour may flag a need for extra support in the new GMC professionalism guidance, Professional behaviours and fitness to practice (GMC, 2016).
Students who are complimented receive a letter detailing the teacher’s comments, together with congratulations from Mr Martin Lupton, Head of Undergraduate Medicine. A copy is saved on the student’s file. The form does not affect progression or ranking and cannot be used as part of the FPAS application. Although students are encouraged to keep forms of this nature as part of their portfolio, you should only complete a compliment form if you feel the student has excelled in some way, and not because the student has suggested it will assist their progress.
The response to the submission of a concern form varies dependent on the issue. Forms go to the Head of Year, year administrator and Deputy Head of Undergraduate Medicine for consideration.
We are always very happy for unprofessional behaviour to be addressed at practices by the teacher (or GP) in question, but it is useful for the School to know about the extent of unprofessional behaviour. It may be that issues such as attendance are recurrent in a student and they require more support from the School, so we encourage you to let us know any issues even if you consider them dealt with.
This is particularly important in the GPPHC course in Year 5, where we are piloting clinical encounter forms in the place of sign-off forms. Although students will get more feedback about their knowledge and skills with the clinical encounter forms, without an end-of-firm sign-off we need you to tell us if anything has been particularly good, or particularly concerning about that student, which can be submitted through the concerns and compliments form system.
GPs who are signing off students will get a link in the confirmatory email they receive from the FEO. The form can always be found here:
https://imperial.eu.qualtrics.com/jfe/form/SV_8CijnFiEtk8UNq5
We also hope to make it available on the College website for easier access in future. Any staff who receive the termly ‘Teaching Bulletin’ will also have access to the standard link.
Thank you again for helping our students and your involvement with this new form.
Dr Joanne Harris
Deputy Head of Undergraduate Medicine

