
We are at a turning point in history: if we fail to change the trajectory of antimicrobial resistance (AMR), by 2050 we face up to 10 million annual global deaths from AMR. Research, solutions, and action in the clinic and at the global political scale are critical to preventing this catastrophe.
To help raise awareness of AMR and highlight the ways that Imperial College London researchers are contributing to the fight against this challenge, the Institute of Infection created three blogs for Antimicrobial Resistance Week, which took place 18th-24th November. The blogs highlighted research at Imperial to understand, manage, and prevent the development of resistance. First, Dr Frances Davies and Dr Elita Jauneikaite explored how resistance develops, looking at the mechanisms used by bacterial pathogens to combat antibiotics and examining AMR at a patient level with preventive measures and novel technologies for tracking and predicting the spread of infection. Dr Gerald Larrouy-Maumus and Dr Jesus Rodriguez Manzano described new diagnostic tools that can rapidly provide clinicians with critical information about resistance and inform decision-making. Finally, Dr Timothy Rawson explained how his group is using artificial intelligence and biosensor technology for precision antimicrobial prescribing, while Dr Nina Zhu described the ongoing work on improving surveillance for infections and AMR.
These are just a few examples of the work of hundreds of Imperial researchers across the disciplines, exploring the origins of AMR and potential solutions at different scales, from the molecular to the systems level. To finish this blog series, we look at a few more examples of AMR research being undertaken at Imperial.
TB and AMR
In the previous blog, Dr Gerald Larrouy-Maumus described his focus on Mycobacterium tuberculosis (TB), which remains one of the top killers worldwide with over 1.5 million deaths per year. Antimicrobial resistance is a serious component of its threat to health, with around half a million people suffering from drug-resistant tuberculosis in 2021, according to WHO. The COVID-19 pandemic saw a rise in inappropriate prescription of antibiotics, and the number of people with drug-resistant TB increased by 3.4% from 2020-2021.
Dr Larrouy-Maumus is not the only one who works on TB and AMR, as we found in our review from March 2023, ‘Meet 7 Imperial researchers working to end TB’. In that piece, Dr Leonid Chindelevitch, from the MRC Centre for Global Infectious Disease Analysis, combines genomics and machine learning to understand how Mycobacterium tuberculosis mutates to develop drug resistance. He understands that eradicating tuberculosis may be difficult, but “what is achievable is significantly reducing the burden of disease that it causes,” and hopes we can “go back to focusing more on tuberculosis and put a stop to the overuse of antibiotics in situations where they are not appropriate. This can be achieved using diagnostics.”
Professor James Seddon (Department of Infectious Disease) explained the impact of resistance on treating tuberculosis in children. “Although we are lucky to be in an age when new antibiotics are being developed, it is disheartening to see resistance develop just as quickly, and the prospect of organisms that are resistant to all known antibiotics is a reality in some rare circumstances, making treatment impossible. However, the only way to completely prevent the development of antibiotic resistance is to not use antibiotics and so there is always a trade-off between responsible use and risk of resistance development.”
Looking at how new diagnostics can contribute to tackling AMR, Dr Ivana Pennisi pointed out, “The diagnosis of infectious diseases such as TB in children is challenging…Diagnostic methods for tuberculosis rely on the cultivation of the causative bacteria, which takes several weeks and usually requires invasive methods for the acquisition of appropriate samples…The urgency for rapid diagnostics tools is further accelerated by the growing threat of drug-resistant tuberculosis”.
“Drug-resistant tuberculosis poses an obstacle that is surely challenging the tuberculosis research clock, intensifying the need for timely and verified data in order to make better-informed decisions to tackle the drug-resistant TB crisis.” – Dr Ivana Pennisi.
Read more about TB and AMR: Meet 7 Imperial researchers working to end TB
Resistant fungal diseases
While most of us think about antimicrobial resistance as a health issue, it also poses major threats to our global food security, environment and ecology, as the Institute of Infection explored in the context of fungi, in our review: ‘How to fight fungal infection: the path of yeast resistance’.
A special problem in the treatment of fungi is that the same antifungal agents are used in human and animal healthcare and agriculture (as well as in other global industries). This dual use accelerates the spread of resistance across the globe and means that we are losing our first line of defence against opportunistic fungal infections in the clinic as well as against crop-destroying fungi, impacting global food systems.
Aspergillus fumigatus can cause the disease aspergillosis in at-risk humans and is a very common mould in soils and air. Fungicides, which are used to protect crops from disease, have led to emerging resistance to antifungal drugs by this mould. A recent citizen science project by Professor Mat Fisher et al. showed that more than 5% of A. fumigatus spores in the UK air are now resistant to the azole antifungals in common use in both the clinic and agriculture. We are all exposed to this mould daily, and this is especially serious for people who are immunocompromised, who are at a greater risk of aspergillosis. “However, it’s not all bad: we’ve recently seen the development of two new highly promising antifungal drugs to which resistance is rare or non-existent” – Professor Mat Fisher.
Imperial researchers, including Professor Darius Armstrong-James and Dr Anand Shah, are also looking at fungal AMR from the clinical perspective. Professor Armstrong-James, who leads the Imperial Fungal Science Network, is looking to immunotherapies as potential treatment options, explaining “[they] are of great potential for infectious diseases such as COVID-19 because of the evolving race that happens between pathogens and their host”. Immunotherapies, therefore, have the potential to avoid antimicrobial resistance. Dr Shah, a Consultant Respiratory Physician and Honorary Clinical Senior Lecturer in the School of Public Health, focuses on ways to combat AMR through improved diagnosis and the use of machine learning and artificial intelligence technologies to understand disease phenotypes, identify patients for stewardship interventions, and integrate complex datasets. He is also working to understand why and how individuals with chronic fungal disease develop antifungal resistance to triazoles (currently the only orally available antifungals) and the source of such resistance
Finally, Dr Johanna Rhodes (School of Public Health) is using a One Health approach to understand fungal infection outbreaks. She uses omics technologies to understand drug resistance mechanisms, transmission events, and how these pathogens spread. Over the last few years, she has become interested in how drug resistance is evolving in a changing climate, where drug-resistant fungi are coming from in the environment and their effect on humans. She has also developed the first genomic surveillance platform for the fungal pathogen Candida auris that will allow clinicians to identify the drug-resistance profile within a few minutes.
Read more about Fungal Science and AMR: How to fight fungal infection: the path of yeast resistance’
Diagnostics to detect antimalarial resistance
The development of drug-resistant malaria parasites poses one of the greatest threats to malaria control and results in increased malaria morbidity and mortality.
“Malaria parasites are very quick to develop resistance to antimalarial drugs, which has posed a continual challenge for malaria treatment, control and elimination. Right now, we have parasites with resistance to our most effective drugs emerging in high-burden countries in Africa, threatening the progress against malaria made over the last two decades”, said Professor Aubrey Cunnington (Department of Infectious Disease).
Professor Cunnington co-leads the NIHR Global Health Research Group on Digital Diagnostics for African Health Systems, which is built around an innovative digital molecular diagnostics device called Lacewing that has the potential to revolutionize access to diagnosis and delivery of treatment in Africa. The technology allows for point-of-care detection of parasite DNA from a few microlitres of blood, with a detection time of 15-20 minutes. Through this programme, the interdisciplinary team that spans continents and expertise in medicine, public health, malaria biology, and engineering aims to address several aspects of antimalarial resistance, including through subprojects focussed on detecting antimalarial resistance at the point of malaria diagnosis.
Read more about the Lacewing platform and how it is being used by the NIHR Global Health Research Group on Digital Diagnostics for African Health Systems.
Comprehensive AMR research expertise
The community of Imperial’s AMR researchers truly covers the breadth of research from the molecular to the global scale. To read more about where research is being undertaken, visit some of the centres and networks with major AMR elements listed below; this is certainly not an exhaustive list. Over the coming year, the Institute of Infection will develop a platform to showcase this portfolio of expertise and will continue to draw researchers together across disciplines to combat this global threat.
- Centre for Bacterial Resistance Biology
- NIHR Health Protection Research Unit in Healthcare Associated Infections and Antimicrobial Resistance
- Centre for Antimicrobial Optimisation
- CAMO-Net: Centres for Antimicrobial Optimisation Network
- MRC Centre for Global Infectious Disease Analysis
- Imperial AHSC: Infection and Antimicrobial Resistance theme
- NIHR Imperial BRC: Infection and AMR theme
- Fungal Science Network of Excellence
- Imperial Malara Network of Excellence
- NIHR Global Health Research Group on Digital Diagnostics for African Health Systems
- B2B2B-AMRDX Network: Bench, bedside, business, and beyond: Innovative solutions for AMR diagnostics
- DIAMONDS network: Rapid diagnostics for better healthcare
- Fleming Centre (Imperial College Healthcare NHS Trust)


 Mary was born in Kingston, Jamaica, in 1805. Her mother was black, and her father was a white army officer. From the age of 12, she helped her mother run a boarding house where they treated sick or injured soldiers, and, at 15, she travelled to England and learned about European medicine. Between 1850 and 1851, Mary nursed victims of cholera epidemics in Kingston and Cruces, Panama, using mustard emetics to make the patient vomit, warm clothes to combat chills, mustard plasters on the stomach and back and calomel in varying doses.
Mary was born in Kingston, Jamaica, in 1805. Her mother was black, and her father was a white army officer. From the age of 12, she helped her mother run a boarding house where they treated sick or injured soldiers, and, at 15, she travelled to England and learned about European medicine. Between 1850 and 1851, Mary nursed victims of cholera epidemics in Kingston and Cruces, Panama, using mustard emetics to make the patient vomit, warm clothes to combat chills, mustard plasters on the stomach and back and calomel in varying doses.  Dr George Rice was born in New York, USA in 1848. After graduating from Dartmouth and training as a surgeon in Edinburgh, he served as a house surgeon at the Royal Edinburgh Infirmary, where he assisted Sir Joseph Lister, the pioneer of antiseptic treatment. Dr Rice then moved to Manchester, worked in the Royal Infirmary as a house physician, and held resident appointments at the Chorlton Union Hospital and Woolwich and Plumstead Infirmary. He also held office under the Metropolitan Asylums Board at the Downs Ringworm Hospital, and was a resident medical officer at the Fulham Workhouse.
Dr George Rice was born in New York, USA in 1848. After graduating from Dartmouth and training as a surgeon in Edinburgh, he served as a house surgeon at the Royal Edinburgh Infirmary, where he assisted Sir Joseph Lister, the pioneer of antiseptic treatment. Dr Rice then moved to Manchester, worked in the Royal Infirmary as a house physician, and held resident appointments at the Chorlton Union Hospital and Woolwich and Plumstead Infirmary. He also held office under the Metropolitan Asylums Board at the Downs Ringworm Hospital, and was a resident medical officer at the Fulham Workhouse.

 Dr Jane Hinton was born in May 1919 in Canton, Massachusetts. Her mother was a teacher, and her father, Professor William Augustus Hinton, was a bacteriologist and one of his era’s most prominent African-American medical researchers. In the 1920s, Augustus
Dr Jane Hinton was born in May 1919 in Canton, Massachusetts. Her mother was a teacher, and her father, Professor William Augustus Hinton, was a bacteriologist and one of his era’s most prominent African-American medical researchers. In the 1920s, Augustus  Professor Dame Elizabeth Nneka Anionwu was born in Birmingham in 1947 and identifies as Irish/Nigerian heritage. She started working for the NHS as a school nurse assistant in Wolverhampton at 16 and was also a health visitor and tutor for the black community in London. In 1979, she helped to establish the first nurse-led UK Sickle & Thalassaemia Screening and Counselling Centre, and from 1990-1997, she worked at the Institute of Child Health, UCL as a Lecturer then Senior Lecturer in Community Genetic Counselling. She later became a Professor and Dean of the nursing school at the University of West London.
Professor Dame Elizabeth Nneka Anionwu was born in Birmingham in 1947 and identifies as Irish/Nigerian heritage. She started working for the NHS as a school nurse assistant in Wolverhampton at 16 and was also a health visitor and tutor for the black community in London. In 1979, she helped to establish the first nurse-led UK Sickle & Thalassaemia Screening and Counselling Centre, and from 1990-1997, she worked at the Institute of Child Health, UCL as a Lecturer then Senior Lecturer in Community Genetic Counselling. She later became a Professor and Dean of the nursing school at the University of West London. Professor Faith Osier studied medicine in Nairobi, Kenya, and while working as a Junior Doctor (1998-2001) in a rural hospital in Kilifi, she would admit up to five children with malaria to the high-dependency unit. Many didn’t survive. This inspired her to think about prevention and how she could stop children from getting malaria in the first place to ‘Make Malaria History’.
Professor Faith Osier studied medicine in Nairobi, Kenya, and while working as a Junior Doctor (1998-2001) in a rural hospital in Kilifi, she would admit up to five children with malaria to the high-dependency unit. Many didn’t survive. This inspired her to think about prevention and how she could stop children from getting malaria in the first place to ‘Make Malaria History’.
 Dr Julia Makinde was born in Delta State, Nigeria, where she obtained her Bachelor’s degree in Zoology from the University of Ibadan. The foundations of her career were established at the University College London and Cardiff University Wales, where she obtained a Master’s degree in Molecular Medicine and PhD in Medicine/Immunology, respectively.
Dr Julia Makinde was born in Delta State, Nigeria, where she obtained her Bachelor’s degree in Zoology from the University of Ibadan. The foundations of her career were established at the University College London and Cardiff University Wales, where she obtained a Master’s degree in Molecular Medicine and PhD in Medicine/Immunology, respectively. 
 Dr Dauda Ibrahim is a postdoctoral research associate in the Clean Energy Process (CEP) Laboratory, Department of Chemical Engineering. He received both his MSc and PhD degrees in Chemical Engineering from the School of Chemical Engineering and Analytical Science, University of Manchester. Dr Ibrahim’s research focuses on the development of systematic frameworks for computer-aided working fluid design and optimisation of organic Rankine cycle systems. Dr Ibrahim also worked on pandemic-response adenoviral vector and RNA vaccine manufacturing. This model-based assessment provides key insights to policymakers and vaccine manufacturers for risk analysis, asset utilisation, directions for future technology improvements, and future epidemic/pandemic preparedness, given the disease-agnostic nature of these vaccine production platforms. He was also first author on ‘Model-Based Planning and Delivery of Mass Vaccination Campaigns against Infectious Disease: Application to the COVID-19 Pandemic in the UK’ paper which showed by integrating demand stratification, administration and the supply chain, the synergy amongst these activities can be exploited to allow planning and cost-effective delivery of a vaccination campaign against COVID-19 and demonstrates how to sustain high rates of vaccination in a resource-efficient fashion.
Dr Dauda Ibrahim is a postdoctoral research associate in the Clean Energy Process (CEP) Laboratory, Department of Chemical Engineering. He received both his MSc and PhD degrees in Chemical Engineering from the School of Chemical Engineering and Analytical Science, University of Manchester. Dr Ibrahim’s research focuses on the development of systematic frameworks for computer-aided working fluid design and optimisation of organic Rankine cycle systems. Dr Ibrahim also worked on pandemic-response adenoviral vector and RNA vaccine manufacturing. This model-based assessment provides key insights to policymakers and vaccine manufacturers for risk analysis, asset utilisation, directions for future technology improvements, and future epidemic/pandemic preparedness, given the disease-agnostic nature of these vaccine production platforms. He was also first author on ‘Model-Based Planning and Delivery of Mass Vaccination Campaigns against Infectious Disease: Application to the COVID-19 Pandemic in the UK’ paper which showed by integrating demand stratification, administration and the supply chain, the synergy amongst these activities can be exploited to allow planning and cost-effective delivery of a vaccination campaign against COVID-19 and demonstrates how to sustain high rates of vaccination in a resource-efficient fashion. 
 To be introduced first is
To be introduced first is 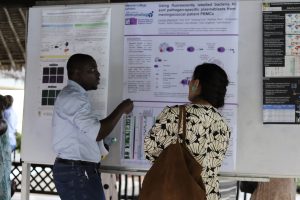 What opportunities would you like ECR to have to help with your careers?
What opportunities would you like ECR to have to help with your careers? The medications used to treat hepatitis C are expensive. This means that many patients living in low- and middle-income countries simply cannot afford the treatment they need. But,
The medications used to treat hepatitis C are expensive. This means that many patients living in low- and middle-income countries simply cannot afford the treatment they need. But, 
 This study found that four interventions – improving blood safety measures, offering drug users more health and safety support, increasing treatment provision, and expanding access to testing – could drastically reduce the number of people contracting hepatitis C. If we adopt these measures, we could meet the WHO target of reducing new hepatitis C infections 80% by 2030. Deaths could be reduced 65% by 2032.
This study found that four interventions – improving blood safety measures, offering drug users more health and safety support, increasing treatment provision, and expanding access to testing – could drastically reduce the number of people contracting hepatitis C. If we adopt these measures, we could meet the WHO target of reducing new hepatitis C infections 80% by 2030. Deaths could be reduced 65% by 2032.