Earlier this June, people at Imperial College London had the opportunity to hear from a scientist who affected all our lives, Professor Dame Sarah Gilbert from the Pandemic Sciences Institute at the University of Oxford. The Department of Life Sciences hosted Prof Gilbert for the Sir Ernst Chain lecture, a celebration of the late biochemist who developed the techniques to isolate and produce Penicillin, together with Howard Florey and Alexander Fleming.
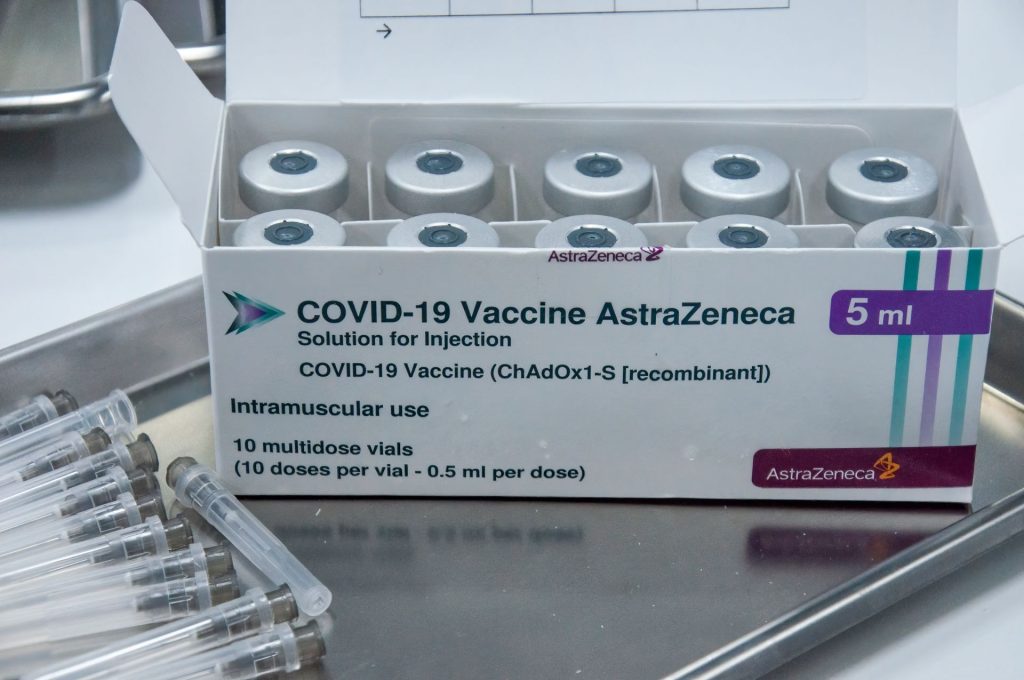
Prof Gilbert works on viral vector vaccines. In 2020 she led the group who, together with Astra Zeneca, developed and produced one of the Covid-19 vaccines. The Oxford/Astra Zeneca (ChAdOx1 nCov-19) vaccine was used in 180 countries. It is estimated to have saved over 6 million lives in the first year it was used!
Our guest blogger, Arabella Heath wrote a blog post about her talk and how combination of molecular science and engineering was crucial for vaccine development in a pandemic.

Vaccine development in a pandemic, the beginning
The Covid-19 vaccine was developed very quickly – human trials started just a few months into the pandemic – thanks to years of prior research into the molecular nature of other viruses. Prof Gilbert started her talk explaining how the 2014 Ebola outbreak in West Africa served as a wake up call. Ebola outbreaks were common but normally limited to rural isolated areas. In 2014, however, the outbreak spread to cities and reached three countries leading to an urgent need to find a vaccine. The world learnt how quickly an epidemic develops and how unprepared we were. There was a feeling that something needed to be done for future epidemics. This led to the World Health Organization (WHO) investing in the development of vaccine platforms to deal with pathogens.
The technology ChAdOx1 at the molecular level
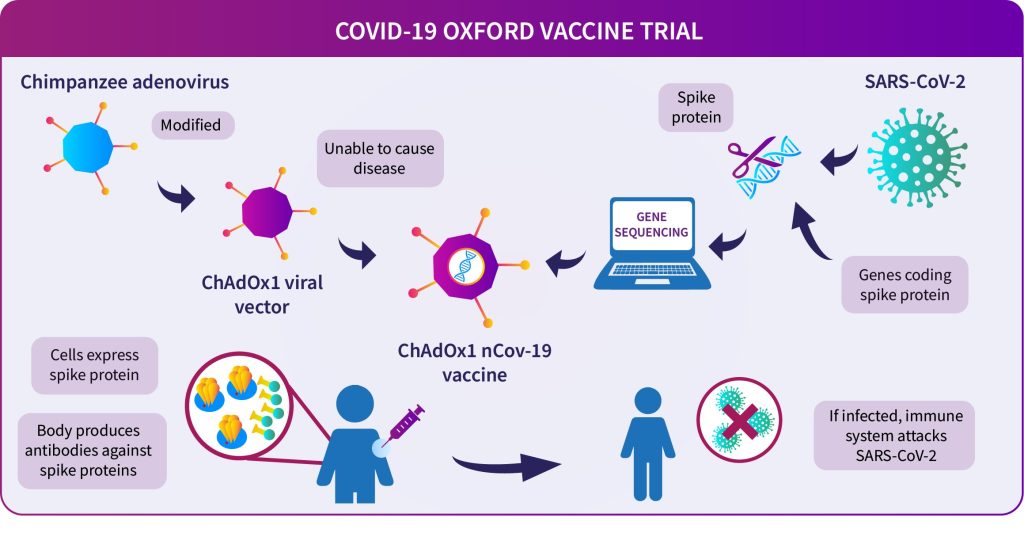
It was then when the Gilbert group developed a new technology called ChAdOx1. ChAdOx1 is a type of a viral vector; a vaccine that sneaks its way into the body in the form of a harmless and genetically modified simian adenovirus. Or, in simpler terms, the chimpanzee variant of an adenovirus (viruses that cause generally minor illnesses, like colds).
The adenovirus is genetically edited to stop it from replicating in the body, and to encode the vaccine antigens (e.g. against Covid-19). Once injected, it infects a cell which then produces the desired vaccine antigens, triggering a strong defensive reaction from the body’s immune system. This allows you to develop immunity to the dangerous virus, without being infected directly.
So, why do we use a chimpanzee virus? Because adenoviruses are so common, many people have antibodies to them. Our immune systems would likely prevent the adenovirus from infecting us, stopping the vaccine from working. Human and chimp viruses are very closely related, so the chimp adenovirus can be used instead.
Manufacturing a vaccine to use globally in the shortest possible time during a pandemic
The readiness of ChAdOx1 technology meant that it could play a crucial role in the Covid-19 vaccination programme. During the UK lockdown, the Oxford-AstraZeneca team worked tirelessly to develop the vaccine. The first trials took place in South Africa and Brazil, places without lockdown because you need an active infection to test the effectiveness. By November 2020, there was evidence that the vaccine worked.
But how do you produce enough quantities of the vaccine? The partnership with Astra Zeneca was initiated in April and they took responsibility for the manufacturing part of the job. Astra Zeneca produced the vaccine in record time, taking just months to roll out the first doses. This aspect required careful engineering to scale up production worldwide. Over 25 manufacturers in 15 different countries produced more than 3 billion doses. Importantly, the vaccine is stable at 4°C making it accessible to people all around the world, regardless of climate.
What can we learn for the future?
Prof Gilbert highlighted how both development of the vaccines but also rapid transfer into manufacturing and clinical trials will be important in the future.
Whilst ChAdOx1 has been successful, Prof Gilbert emphasised the importance of monitoring emerging pathogens, many of which do not yet have approved vaccines. She also discussed crucial issues concerning vaccine development. These include the ethics of running trials during deadly epidemics, scaling up vaccine production, and developing vaccines for viruses with different lineages. These points re-enforced the importance of continuing to invest money in medical research and education. The new Pandemic Sciences Institute in Oxford will use information from Covid-19 to identify and prevent future pandemics, focusing on equitable access to medical innovation.