What have we been up to?
Over the last few months we have been finalising the report of our research with the NHS RHO comparing inequalities in sickle cell with cystic fibrosis and haemophilia. We have kept you up-to-date on the progress of our work and we are pleased to announce that our report has been published and can be accessed here.
1. Word Sickle Cell Day 2025
 Today is World Sickle Cell Day, an initiative started in 2009 following a 2008 resolution by the United Nations’ General Assembly recognising that sickle cell disease was a publc health problem and urging member states to raise more awareness of this neglected genetic condition.
Today is World Sickle Cell Day, an initiative started in 2009 following a 2008 resolution by the United Nations’ General Assembly recognising that sickle cell disease was a publc health problem and urging member states to raise more awareness of this neglected genetic condition.
The UK Sickle Cell Society has a campaign to “Tell it out loud“. Please help us to amplify awareness of this neglected disease through one or more actions suggested by the Society, including sharing your story or giving blood.
2. Launch of Sickle Cell Comparative Report to inform policy

Today, we will be presenting our comparative sickle cell research project in the House of Lords to mark the launch of our report with the NHS RHO. Our work comprised of a literature review, an analysis of specific indicators related to inequality, a study comparing hospital admissions data and a survey on experiences of inequalities among people with lived experience of sickle cell.
Our key findings from this work included:
- 2.5 times more research funding per person for cystic fibrosis than for sickle cell or haemophilia
- 42% increase in hospital admissions for sickle cell between 2013 and 2022
- Total estimated annual hospitalisation costs two times higher for sickle cell than cystic fibrosis
- Around 2 specialist nurses per 100 patients for cystic fibrosis vs ~0.5 for sickle cell
- On average, patients with sickle cell managed 7 pain crises without medical help
Our key recommends focused on:
1. Better Data
- To improve data access and use
- To drive accountability through data
2. Better Support
- Fund Action-Focused Research
- Strengthen Workforce Education
3. Better Treatment
- Ensure Access to Curative Therapies
- Embed Equity in Clinical Guidelines
2. Other updates
- Sickle cell community engagement event with NIHR, Genomics England and Imperial Healthcare NHS Trust
In March, Rutendo volunteered at an event to focused on engaging with the sickle cell community on research. A video of the event can be viewed on youtube below.
Engagement with sickle cell community on research
- Global Congress on Sickle Cell Disease
 The 5th Global Congress on Sickle Cell Disease was hosted earlier this month in Abuja, Nigeria. This was really symbolic as Nigeria is the country with the largest burden of sickle cell disease. It was an opportunity to hear about the latest development in research, treatments and policies from a wide range of stakeholders.
The 5th Global Congress on Sickle Cell Disease was hosted earlier this month in Abuja, Nigeria. This was really symbolic as Nigeria is the country with the largest burden of sickle cell disease. It was an opportunity to hear about the latest development in research, treatments and policies from a wide range of stakeholders.
 Rutendo volunteered in planning and delivering a
Rutendo volunteered in planning and delivering a 

 This month ended with groundbreaking news as the gene therapy for sickle cell
This month ended with groundbreaking news as the gene therapy for sickle cell  Earlier this month, Rutendo attended a public engagement event at The Healing Church of God in Christ (THCOGIC) in London. Dr Steven Okoli led a talk raising awareness of sickle cell and Rutendo discussed our current and future research on sickle cell with the congregation. It was great to see the congregation’s enthusiasm and motivation to raise awareness of sickle cell.
Earlier this month, Rutendo attended a public engagement event at The Healing Church of God in Christ (THCOGIC) in London. Dr Steven Okoli led a talk raising awareness of sickle cell and Rutendo discussed our current and future research on sickle cell with the congregation. It was great to see the congregation’s enthusiasm and motivation to raise awareness of sickle cell. In February (20th and 27th) and March (6th),
In February (20th and 27th) and March (6th), 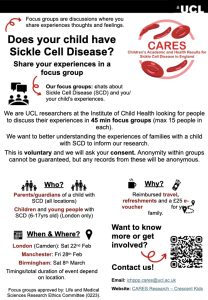 Researchers at the Institute of Child Health at UCL and
Researchers at the Institute of Child Health at UCL and 

 On Friday 25th October, Fred delivered a presentation on his sickle cell research at the launch event of the Sickle Cell Alliance at Imperial College London hosted by the Imperial Sickle Cell Group and Imperial Enterprise. The alliance seeks to build collaborative partnerships on sickle cell across faculties, institutions, and industries while informing national policy.
On Friday 25th October, Fred delivered a presentation on his sickle cell research at the launch event of the Sickle Cell Alliance at Imperial College London hosted by the Imperial Sickle Cell Group and Imperial Enterprise. The alliance seeks to build collaborative partnerships on sickle cell across faculties, institutions, and industries while informing national policy. conducted by University College London’s
conducted by University College London’s 


 On 27th June this year, the hit show Supacell premiered on Netflix. The superhero drama, created and produced by Andrew Onwubolu (known as Rapman), follows a group of black Londoners who develop superpowers triggered by sickle cell. Rapman told
On 27th June this year, the hit show Supacell premiered on Netflix. The superhero drama, created and produced by Andrew Onwubolu (known as Rapman), follows a group of black Londoners who develop superpowers triggered by sickle cell. Rapman told