Tiny Airways, Big Impact
The damage of the small airways of the lungs can result in inflammation, structural changes, and increased airway resistance. This is a common characteristic of chronic respiratory diseases such as asthma or chronic obstructive pulmonary disease (COPD). While the small airways of the lungs may not be the star of the show, they are a crucial part of the lung health story.
Spirometry: The Lung Detective
Small airways obstruction (SAO) can be detected using spirometry. Traditionally, the mean forced expiratory flow rate between 25% and 75% of the forced vital capacity (FEF25-75) is the preferred parameter. However, novel parameters such as the forced expiratory volume in 3 seconds as a ratio of the forced expiratory volume in 6 seconds (FEV3/FEV6), have proven effective at detecting SAO.
We know that chronic respiratory diseases are leading causes of mortality around the world. Can SAO, even without ticking all the boxes for a doctor diagnosis of respiratory disease, predict death?
The big UK Biobank Study: What did we find?
We analysed the data of over 250,000 participants from the UK, who had high quality spirometry, and found some novel results:
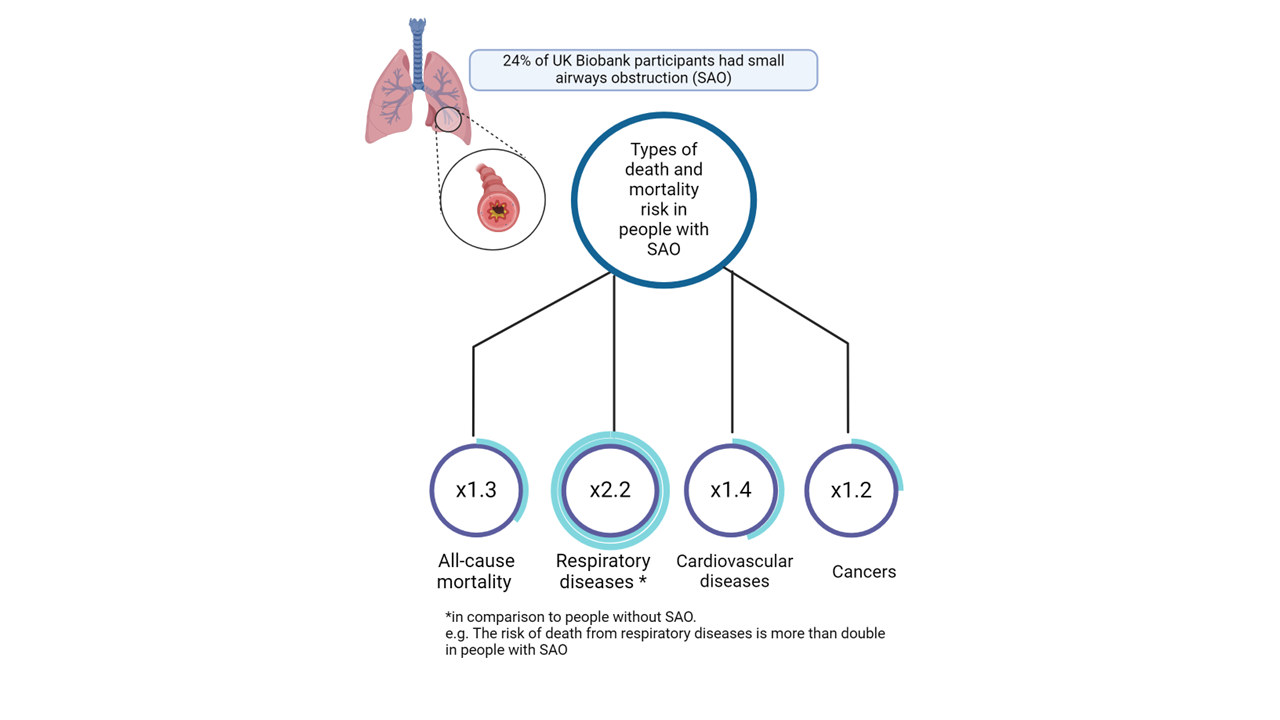
- About 24% of participants had SAO. Among these, about 10% had isolated SAO, meaning their small airways were obstructed, but their larger airways were not.
- People with SAO had increased risk of death from all causes, including respiratory diseases, cardiovascular diseases, and cancers. The risk was especially high for respiratory diseases, with more than double compared to those without SAO.
- Even without respiratory disease (isolated SAO), the mortality risk was increased for cardiovascular diseases and cancers. Importantly, these findings were also true among people who have never smoked, indicating that SAO itself, regardless of smoking, is a critical factor.
Mortality risk in people with small airways obstruction
Why should we care?
- Early Detection: Catching SAO early could be crucial in preventing more severe lung diseases later in life.
- Lifestyle Factors: Smoking is a big no-no for lung health, but even people who have never smoked can have SAO. This is likely to be caused by other factors.
While the UK Biobank cohort’s lack of representativeness and the relatively short follow-up period pose limitations, the study’s large sample size adds significant weight to the findings. Future research should aim to replicate these results in more diverse populations and explore the underlying mechanisms linking SAO to increased mortality.
Take home message.
Understanding and detecting SAO can give us a head start in managing chronic respiratory diseases such as COPD and asthma. Ultimately, this can aid to reduce respiratory morbidity worldwide. The findings of this study were published in the peer-reviewed journal CHEST. The article can be freely accessed and read here: https://doi.org/10.1016/j.chest.2024.04.016