by Dr Nicky Hawkins, Dr Nina Dutta, Dr Neepa Thacker and Dr Arti Maini
The Undergraduate Primary Care Education Team leads on the delivery of a wide range of courses across the six years of the Imperial MBBS programme. On March 14th 2020, the medical school announced the suspension of all face-to-face undergraduate clinical placements in light of the COVID-19 pandemic. With major implications for two of our key primary care courses – Year 3 Medicine In the Community Apprenticeship (MICA) and Year 5 General Practice and Primary Healthcare (GPPHC) – we were tasked with the rapid conversion of these face-to-face clinical attachments into courses that could be developed and delivered entirely remotely.
Traditionally, both MICA and GPPHC are centred around medical students observing and assisting doctors in an authentic clinical environment, regularly engaging in meaningful interactions with patients themselves. The team therefore sought to capture the complexities of this learning environment, ensuring that we were adequately addressing the educational needs of our students. Here we describe and reflect on selected key components of the digital MICA and GPPHC courses, sharing some of the lessons learned from our students along the way.
Large group live webinars. Alongside other webinars, both MICA and GPPHC digital courses incorporated weekly live ‘Case Rounds’; webinars centred around clinical cases and questions, circulated to students in advance. Attended by up to 140 students, interactivity was integral to these webinars and maintained by actively encouraging students to submit questions and answers via the ‘chat’ and utilising real-time voting applications such as Mentimeter. Student feedback on live webinars in general was overwhelmingly positive. It was interesting to hear them repeatedly describe feeling liberated to interact more freely, due to the anonymity of the online format; it appeared to create a more inclusive environment for students whilst retaining engagement and learning value.
“I like this format because I feel more comfortable to engage and interact compared to face to face. Makes it feel safe knowing that we can contribute without other students knowing it’s me giving that answer…I felt more engaged and switched off less. I think it’s a good idea which should be incorporated more for future years.” Year 3 MICA student
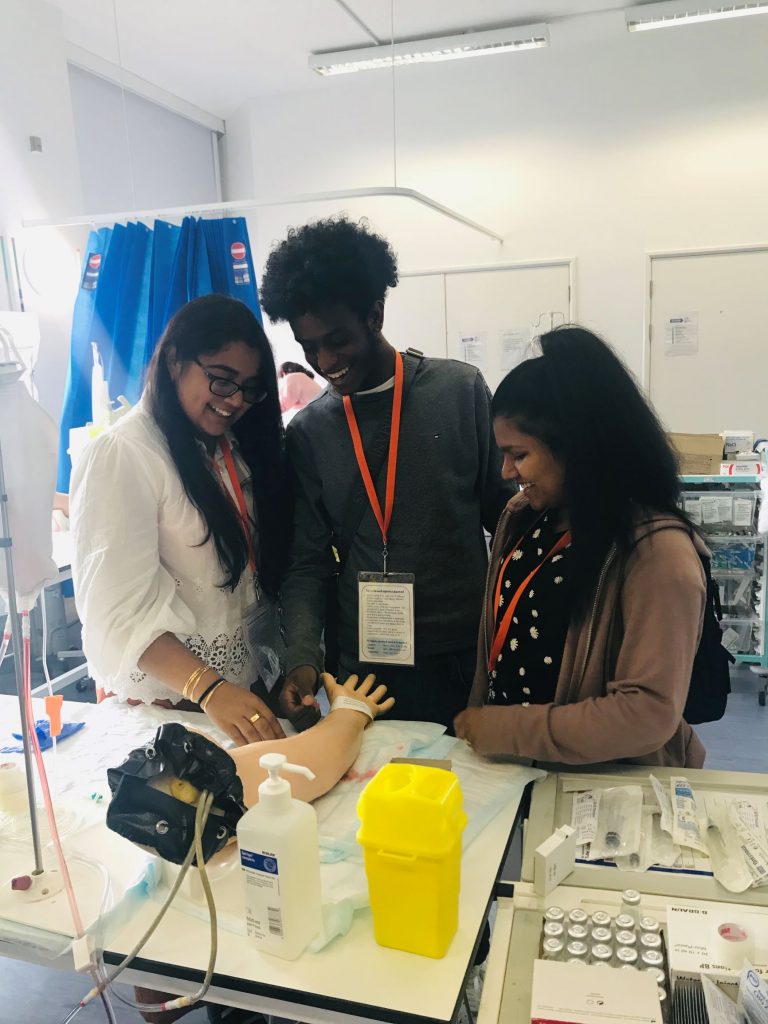
Small-group history taking sessions. Recognising the need for peer-peer interaction, and a platform to actively promote development of students’ consultation skills, both MICA and GPPHC held history taking sessions using Zoom’s breakout room function to facilitate interactive small-group work. This enabled role-play of a range of primary care scenarios. Students rated the session highly, commenting on the value of real-time personalised feedback from both tutors and their peers.
“It was a good opportunity to socially connect with colleagues remotely and undertake some peer-to-peer learning.” Year 5 GPPHC student
Self-study e-learning resources. Alongside timetables of live sessions, an online package of learning materials mapped to core curriculum content was made available to both MICA and GPPHC cohorts, combining internally created resources and external resources that had been quality assured by the team. Well received by students, this was available to access remotely in their own time, at their own pace, promoting asynchronous online learning.
As a team, we have rapidly upskilled in our digital capabilities to deliver innovative online learning across a range of formats. It is exciting to pause and reflect on what has been achieved in such a short space of time. We have also had the opportunity to collaborate with colleagues in Melbourne University who have been leading a similar radical change to digital delivery of medical education. This collaboration has led to shared learning and innovation, which has led to a acceptance of a joint publication in The Clinical Teacher.
Drawing on the valuable lessons learned, we are looking to develop these digital course components further as we approach the start of the new academic year. Although students will be returning to clinical placements, it is clear there will remain an important role for digital learning strategies alongside more traditional placement teaching.