Depression and anxiety are the most common mental health illnesses, affecting 264 million and 284 million people worldwide, respectively – equivalent to 3.4% and 3.8% of the global population. However, it’s thought that many cases are unreported – the real figures are expected to be double what is recorded. What’s going on at a molecular level in the brain during depression and anxiety? How does medication change this?
by Naveesha Karunanayaka, Kieran Brophy and Steph Pendlebury
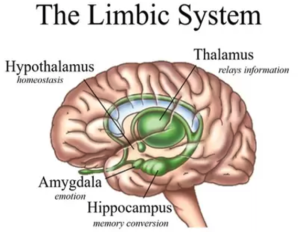
Despite increased understanding of mental health illnesses, there is still a lack of quantitative measures to diagnose them. Although closely related, anxiety is associated with a high-energy state, whereas depression is thought of as a low-energy state. They are both thought to result from disruption to emotional centres in the brain, namely the amygdala, hippocampus and other components of the pre-frontal cortex. Both illnesses relate to a lack of chemical regulation in these areas leading to an imbalance of chemicals in the brain, which impacts an individual’s response to various situations. Different areas of the brain show vulnerability at different stages of life. Environmental impacts, such as traumatic and experiences or chronic stress over an extended period of time, can result in depression or anxiety.
Depression
The science behind depression
The areas in the brain that are known to play a significant role in depression are the amygdala, thalamus and hippocampus (see Figure 1). Using sophisticated brain imaging techniques, studies have shown that the hippocampus is 9% to 13% smaller in certain people suffering from depression. Experts believe that stress can suppress the production of new neurons (nerve cells) in the hippocampus, making it smaller. This happens due to shrinkage of dendrites, which is where a neuron receives input from other cells, and loss of spines in the neurons. Although antidepressants immediately increase the number of neurotransmitters in the brain, many people don’t feel better for a couple of weeks or more. This could be because mood only improves once there has been new nerve growth, which allows new connections, but this takes time. So, the important effect of these medications may be in generating new neurons.
Molecular origins
Neurotransmitters are molecules used by the nervous system, which act between neurons, to transmit messages across the body. These play an essential role in regulating mood; they can either inhibit or activate the neuron at which they arrive. They also affect the initial neuron that released the neurotransmitter. This is because a feedback mechanism reabsorbs the excess neurotransmitters into the cell; the excess is broken down by enzymes. However, when this system fails, it can lead to increased or decreased sensitivity in the receptor neuron, or the emitting neuron may generate too much or too little neurotransmitter. This chemical imbalance is a common cause of depression.
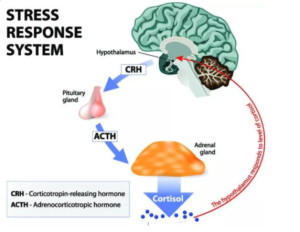
Stress can also play a key role in depression. The stress response signal originates from the hypothalamus, which is linked to both the pituitary and adrenal glands forming the hypothalamic-pituitary-adrenal (HPA) axis (Figure 2). When a threat is detected, the hypothalamus releases a hormone called the Corticotropin-Releasing Hormone (CRH), which stimulates the body by causing the adrenocorticotropic hormone (ACTH) to be released into the bloodstream. This combined release of hormones culminates in the release of cortisol. Usually, once a certain blood concentration of cortisol is reached, alleviating the stressor, a negative feedback mechanism between the cortisol, CRH and ACTH occurs, bringing the level of cortisol is back down to a normal level.
Dysfunction of the HPA axis is linked to mental disorders, via increased levels of CRH and cortisol. This occurs when the body detects ongoing stressors, resulting in a continuous stress response. The body becomes accustomed to this heightened level of stress and increased levels of cortisol. Consequently, the negative feedback system breaks down and the cortisol level rises in the body as more and more CRH and ACTH is produced, creating a cycle of increasing stress.
Prolonged exposure to high cortisol can cause atrophy (the progressive degeneration of muscle or other tissue) of the hippocampus and hypertrophy (increased size) of the amygdala. High cortisol levels induce exhaustion, and can also affect other neurotransmitters, such as causing depletion of serotonin. Selective serotonin reuptake inhibitors (SSRIs) are often used to restore full activity of serotonin in an individual with depression.
Anxiety
The science of anxiety
The amygdala and hippocampus also play a key role in anxiety and mood regulation. The amygdala is responsible for detecting observable external emotional stimuli and initiating a suitable behavioural response. It deals mainly with fear, aggression and defensive behaviour, as well as the retrieval of memories related to these emotions. Although “anxiety” and “fear” are sometimes used interchangeably, evidence suggests that there are different molecular mechanisms underlying these emotions.
Molecular causes of anxiety
Fear is a fight-or-flight response to an identifiable, immediate threat. Anxiety, however, is a prolonged apprehension around uncertain events that do not pose an imminent threat. Amygdala lesions, areas where the amygdala is damaged due to illness or invasive surgery, tend to block the fear response but not prolonged anxiety states. The reason for this difference could be because the central amygdala may be involved with processing cues relating to fear, while information regarding anxiety is processed elsewhere. However, this is beginning to be contested.
Anxiety disorders develop when the activity of the amygdala increases past normal levels and becomes uncontrollable; the amygdala overreacts to situations that aren’t actually threatening. Some research suggests that different regions of the amygdala are activated in different anxiety disorders. However, we know that the central amygdala has primary control of all anxiety-related behavioural responses. Lesions in the central amygdala cause decreased levels of the hormones CRH and ACTH. Consequently, the levels of these hormones are too low to release cortisol into the bloodstream, so stress is not alleviated.
The amygdala also receives input from other regions of the brain: the hippocampus, thalamus and hypothalamus. The molecular mechanisms of the hypothalamic-pituitary-adrenal (HPA) axis, linked to depression, also play a role in anxiety. Long-term increased levels of CRH and cortisol make the HPA axis hypersensitive, causing a cycle of constant stress and worry. In addition, the volume and neurogenesis (the biological process of nervous tissue growth) of the hippocampus are related to stress sensitivity and stress response. Smaller sized hippocampi, linked with depression, may generate stronger anxiety symptoms. Lesions in the hippocampus may prevent the ability to avoid stressful stimuli. Sustained levels of stress over an extended period of time have been linked with neuron growth suppression in the hippocampus, which is a key factor in anxiety and depression.
Treatment
Currently, some of the most common forms of treatment for depression and anxiety are psychotherapy or cognitive behavioural therapy (CBT), which is talk therapy, and pharmacotherapy – the use of medication.
Use of medication
Several different medication options are available; however, all may result in side effects of different severity. The first line of medications used for both anxiety and depression are usually selective serotonin reuptake inhibitors. These are better tolerated in the case of overdose, and have relatively positive benefit/risk balance in comparison to alternatives. Benzodiazepine is sometimes used, however, treatment using this drug could lead to central nervous system damage, as well as impairment in cognitive function and other side effects. Often preference to newer alternative drugs is given over benzazepine based on the known risks of its use, rather than the merit of the other drugs. Proper risk/benefit analysis for any medication is essential.
Second line treatments for both disorders are usually tricyclic antidepressants (TCAs), however, adverse effects are much more frequent, and they are very toxic in the case of overdose. Therefore, these drugs are not advised to be used with suicidal patients.
A key research challenge is to understand the molecular nature of these drugs’ effects – good and bad – so that better, more targeted treatments can be developed.
Incorporating Cognitive Behavioural Therapy

Cognitive behavioural therapy (CBT) is an intervention for psychiatric disorders such as depression and anxiety disorders. It tackles the inner beliefs of the patient (Figure 3), however, the neural mechanisms of action behind it are unclear. It is one of the most effective treatment strategies for anxiety and depression and provides a significantly better outcome when it’s combined with pharmacotherapy, compared to the use of pharmacotherapy alone. Relapse rates are also much lower when using a combination of CBT and pharmacotherapy.
Psychotherapy is recommended and accepted as an effective treatment used commonly for mild to moderate episodes. However, areas of the world that do not have enough qualified therapists are limited to the use of pharmacotherapy on its own as the first line of treatment.
Conclusions
Anxiety and depression have a lot in common in terms of symptoms, diagnosis and treatment. A precursor for both illnesses is clearly stress, through the action of the HPA axis, regulating the release and feedback of certain hormones, which has a huge impact on the composition of the amygdala and hippocampus. The negative feedback system of the HPA axis on cortisol and stress plays a major role in both illnesses. Equally important are neurotransmitters, such as serotonin and CRH, that work to reduce stress states and promote mood regulation. Treatment of anxiety and depression is not clear-cut, and not without side-effects. The current best treatment option is first-line medications, such as SSRIs, combined with cognitive behavioural therapy – this provides chemical balance and mental strength. The molecular basis of the benefit of CBT is not yet understood.
This is part of a blog series on the molecular science of mental health. Coming up next: schizophrenia, diagnostic tools and digital twins.
Further reading
Alschuler, L. (n.d.). HPA Axis & Stress Response: Hypothalamic Pituitary Adrenal Axis. Available from: https://www.integrativepro.com/articles/the-hpa-axis [Accessed 11th July 2021].
Bandelow, B., Michaelis, S., & Wedekind, D. (2017). Treatment of anxiety disorders. Dialogues in clinical neuroscience, 19(2), 93–107. doi: https://doi.org/10.31887/DCNS.2017.19.2/bbandelow
Boyle, M. (2020). The Amygdala and the emotional brain: when fear overrides the rational. Available from: https://www.vitawell.com.au/blog/the-amygdala-and-the-emotional-brain–when-fear-overrides-the-rational- [Accessed 20th July 2021].
Duval E, Javanbakht A, Liberzon I. Neural circuits in anxiety and stress disorders: a focused review. Therapeutics and Clinical Risk Management. 11:115-126. doi: https://doi.org/10.2147/TCRM.S48528.
Fenn, K. and Byrne, M. (2013). The key principles of cognitive behavioural therapy. InnovAiT. 6(9): 579-585. doi: https://doi.org/10.1177%2F1755738012471029
Harvard Medical School (n.d.). What causes depression? Available from: https://www.health.harvard.edu/mind-and-mood/what-causes-depression [Accessed 10th July 2021].
Irle, E., Ruhleder, M., Lange, C., Seidler-Brandler, U., Salzer, S., Dechent, P., Weniger, G., Leibing, E., Leichsenring, F. (2010). Reduced amygdalar and hippocampal size in adults with generalized social phobia. Journal of Psychiatry & Neuroscience.35(2): 126–131. doi: 10.1503/jpn.090041.
Knapp, S. (2020). HPA Axis. Available from:https://biologydictionary.net/hpa-axis/ [Accessed 26th December 2021].
Linsambarth, S., Moraga-Amaro, R., Quintana- Donoso, D., Rojas, S. and Stehberg, J. (2017). The Amygdala and Anxiety. doi: 10.5772/intechopen.68618.
Martin, E.I, Ressler, K.J., Binder, E., Nemeroff, C.B. (2009). The Neurobiology of Anxiety Disorders: Brain Imaging, Genetics, and Psychoneuroendocrinology. Psychiatric Clinics of North America. 32(3): 549–575. doi: 10.1016/j.psc.2009.05.004.
Ritchie, H. and Roser, M. (2018) – “Mental Health”. Published online at OurWorldInData.org. Available from: https://ourworldindata.org/mental-health [Accessed 9th July 2021].
Stephens, M.A.C., Wand, G. (2012). Stress and thee HPA axis. Alcohol Research. 34(4): 468–483. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860380/ [Accessed 11th July 2021].