Schizophrenia is a chronic mental illness affecting around 20 million people worldwide and is most common in young men (according to the World Health Organisation). How are the tools of genetics and AI being used to improve treatment?
By Naveesha Karunanayaka
Schizophrenia often causes an individual to have skewed perceptions, in the form of hallucinations, disorganised thoughts and speech, and lack of motivation. Although little is known about the exact causes of schizophrenia, it clusters in families and is thought to be caused by genetic rather than cultural or environmental factors.
There have been developments in the area through the study of genetics and a molecular approach, as well as more recent progress using artificial intelligence (AI). The molecular mechanisms for the prevalence and differences in the disease between the sexes are not yet fully understood, but one hypothesis suggests a link to the early development of the neuronal system.
If we can better understand the molecular-level causes of the disease, we will be better placed to find new, more effective treatments. One early hypothesis proposed that schizophrenia was due to the hyperactivity in dopamine transmission. However, with the ability to study genetics at a molecular level this was found to be less relevant – genetic variations play a major role.
Molecular approaches
In the molecular approach, methods such as “Linkage Analysis” are used. This tests the tendency of groups of genes on a chromosome to be inherited together. The association method then tests whether a genetic deviation within one of those genes is associated with a certain disease.
Linkage analysis of schizophrenia found evidence for two different locations of interest, based on different types of the disease. Initially certain chromosomes seemed to be related to disorganised schizophrenia and paranoid schizophrenia, but studies of large numbers of people did not find a statistically significant effect. So whilst linkage studies have been somewhat successful for some non-psychiatric diseases, particularly those that have a defined genetic trait passed through generations, it has not yet been possible to identify any specific genes linked to psychiatric disorders.
The association method is far more powerful. It specific genes that are thought to be involved in a certain disease, called “candidate genes”, are investigated. Two similar study groups are used, one containing people with the disease and the other without. Researchers collect DNA samples from each participant. Each person’s DNA is surveyed for genetic markers related to variation of the candidate genes. If a certain genetic variation is found to appear more frequently in participants with the disease, compared to those without, this variation is said to be “associated” with the disease.
An added complication is that the associated genes may not actually be causing the disease, they may just be “tagging along” with the gene variants that are responsible for the disease. So additional steps are required to pinpoint the exact genetic cause of the disease.
So far, association studies have been successful in finding areas of interest for schizophrenia, such as the major histocompatibility complex (MHC) region in mice (the equivalent for humans is the Human Leukocyte Antigen (HLA)), transcription factor 4 (TCF4) and neurogranin (NRGN). These results have been successfully corroborated through other independent studies. However, a serious limitation to the research to date is that it is usually limited to Western populations. One study conducted with Han Chinese participants found a previously unknown variation that could cause schizophrenia in this particular population. This indicates the importance of studying diverse groups of participants.
New computer-aided research tools
Artificial Intelligence (AI) and physical devices
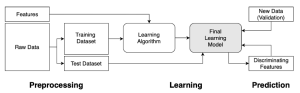
Advancements in artificial intelligence (AI), new machine learning techniques and algorithms have enabled important breakthroughs. For example, key proteins in a N-methyl-D-aspartate receptor (NMDAR) pathway have been related to schizophrenia. It is thought that individuals with excess of these key proteins reduce the NMDAR activity, resulting in schizophrenia. There are some suggestions that melatonin, a hormone that regulates our sleep cycle, is also linked to schizophrenia. However, more research is required to determine whether there is a direct causal link between melatonin levels and schizophrenia.
AI can also assist diagnosis, enabling earlier, more accurate detection. It can be used to analyse various types of scans, such as MRI (magnetic resonance imaging), PET (positron emission tomography), and EEG (electroencephalogram). AI has also been developed for use in a novel evidence-based tool to detect certain neural signals in the brain by analysing an image from an MRI scan. Machine learning is also being harnessed to develop predictive models depending on variables such as family history, age, and sex.
Treatments
Effective treatments require a molecular-level understanding of the disease, which we currently don’t have, so, a cure for schizophrenia has not yet been developed. But often immediate treatment after the first episode is crucial.
First generation drugs act on the dopamine system, while second-generation medicines (such as olanzapine, amilsulpride and risperidone) target serotonin receptors. Second generation antipsychotic drugs are preferred as first line therapy as they have fewer neurological side effects and are associated with fewer drug-induced movement disorders.
Psychotherapy is also used alongside pharmacotherapy (medicines) to aid progress and help patients return to normal life.
Future developments
In 2021, a project was launched to investigate new treatments for schizophrenia, funded by the Psychiatry Consortium. Several large pharmaceutical groups, research charities and academic institutes will contribute. They will use a newly designed technical approach to assess which proteins are selectively produced by a gene related to schizophrenia, and how this differs from other human tissues. From this, it may be possible to identify promising drug targets for schizophrenia treatment.
Conclusions
Developments in schizophrenia research aren’t conclusive and lack definitive loci, making it hard to home in on one area to research further and pursue as a root cause. However, the molecular-level understanding of the illness and the genes associated with it is now improving. We now know that genetic variations have the greatest effect, although there is still much more to learn about how they lead to the illness developing. The success of early AI and machine learning developments to detect, analyse, diagnose, and predict factors relating to schizophrenia is a hopeful avenue for the future. It is extremely important that different population groups are studied, as results to date are mostly only relevant to Western populations.
With the advancement in the technological sector, hopefully schizophrenia research will be catalysed, and tools such as AI can be used effectively to find a cause and a cure for the illness. In the next blog we will explore other diagnostic tools for mental health, such as smart devices, brain-computer interfaces and a more detailed look into AI.
Explore more with Imperial
This is a part of a blog series about molecular science in mental health. Read more about depression and anxiety, diagnostic tools, and digital twins here!
Further reading
Avramopoulos D. (2018). Recent Advances in the Genetics of Schizophrenia. Molecular Neuropsychiatry. 4:35-51. doi: 10.1159/000488679.
Berry, N., Jobanputra, V. and Pal, H. (2003). Molecular genetics of schizophrenia: a critical review. Journal of psychiatry & neuroscience : JPN, 28(6), 415–429. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC257788/ [Accessed 25th July 2021].
Bulayeva, K.B., Glatt, S.J., Bulayev, O.A., Pavlova, T.A. and Tsuang, M.T. (2007). Genome-wide linkage scan of schizophrenia: A cross-isolate study. Genomics. 89(2):167-177. https://doi.org/10.1016/j.ygeno.2006.10.001
Earlham Institute (2021). Investigating new treatment for schizophrenia as first Psychiatry Consortium funded project announced. Available from: https://www.earlham.ac.uk/newsroom/investigating-new-treatment-schizophrenia-first-psychiatry-consortium-funded-project [Accessed 4th August 2021].
Flanagan, R.J., Lally, J., Gee, S., Lyon, R. and Every-Palmer, S. (2020). Clozapine in the treatment of refractory schizophrenia: a practical guide for healthcare professionals. British Medical Bulletin, 135(1):73-89. doi: https://doi.org/10.1093/bmb/ldaa024
Guzman, F. (2019). First vs Second-Generation Antipsychotics. Available from: https://psychopharmacologyinstitute.com/publication/first-vs-second-generation-antipsychotics-2082 [Accessed 1st August 2021].
Lai, J.W., Ang, C.K.E., Acharya, U.R., and Cheong, K.H. (2021). Schizophrenia: A Survey of Artificial Intelligence Techniques Applied to Detection and Classification. International Journal of Environmental Research and Public Health. 18(6099): 1-20. doi: https://doi.org/10.3390/ijerph18116099
Lin, E., Lin, C.-H., Hung, C.-C., and Lane, H.-Y. (2020). An ensemble approach to predict schizophrenia using protein data in the N-methyl-D-aspartate receptor (NMDAR) and tryptophan catabolic pathways. Frontiers in Bioengineering and Biotechnology. 8(569): 1-7. doi: 10.3389/fbioe.2020.00569
Mokhtari, R. and Lachman, H. M. (2016). The Major Histocompatibility Complex (MHC) in Schizophrenia: A Review. Journal of clinical & cellular immunology. 7(6): 479. https://doi.org/10.4172/2155-9899.1000479
National Human Genome Research Institute (n.d.). Genome-Wide Association Studies Fact Sheet. Available from: https://www.genome.gov/about-genomics/fact-sheets/Genome-Wide-Association-Studies-Fact-Sheet [Accessed 27th July 2021].
Nieratschker V, Nöthen M.M. and Rietschel M. (2010). New genetic findings in schizophrenia: is there still room for the dopamine hypothesis of schizophrenia? Frontiers in Behavioural Neuroscience. 4(23): 1-6. doi: 10.3389/fnbeh.2010.00023.
University of Alberta Faculty of Medicine & Dentistry (2021). AI used to predict early symptoms of schizophrenia in relatives of patients. Available from: https://www.sciencedaily.com/releases/2021/01/210126171642.htm [Accessed 3rd August 2021].
World Health Organisation (2019). Schizophrenia. Available from: https://www.who.int/news-room/fact-sheets/detail/schizophrenia [Accessed 23rd July 2021].
Yue, W., Yu, X. and Zhang, D. (2017). Progress in genome-wide association studies of schizophrenia in Han Chinese populations. npj Schizophr 3(24): 1-9. doi: https://doi.org/10.1038/s41537-017-0029-1.