- My Imperial Global Development Fellows Fund Placement at Imperial
- Researchers and community members working together to shape research on respiratory infections in young children
- HOPE for Hand Osteoarthritis
- Having an Impact with Public Involvement in Paediatric Intensive Care Research
- Public engagement and involvement at the Cardiomyopathy UK conference: When researchers and the public meet
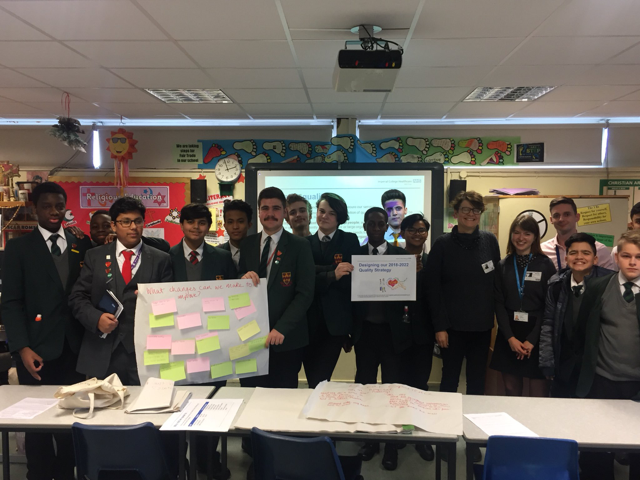
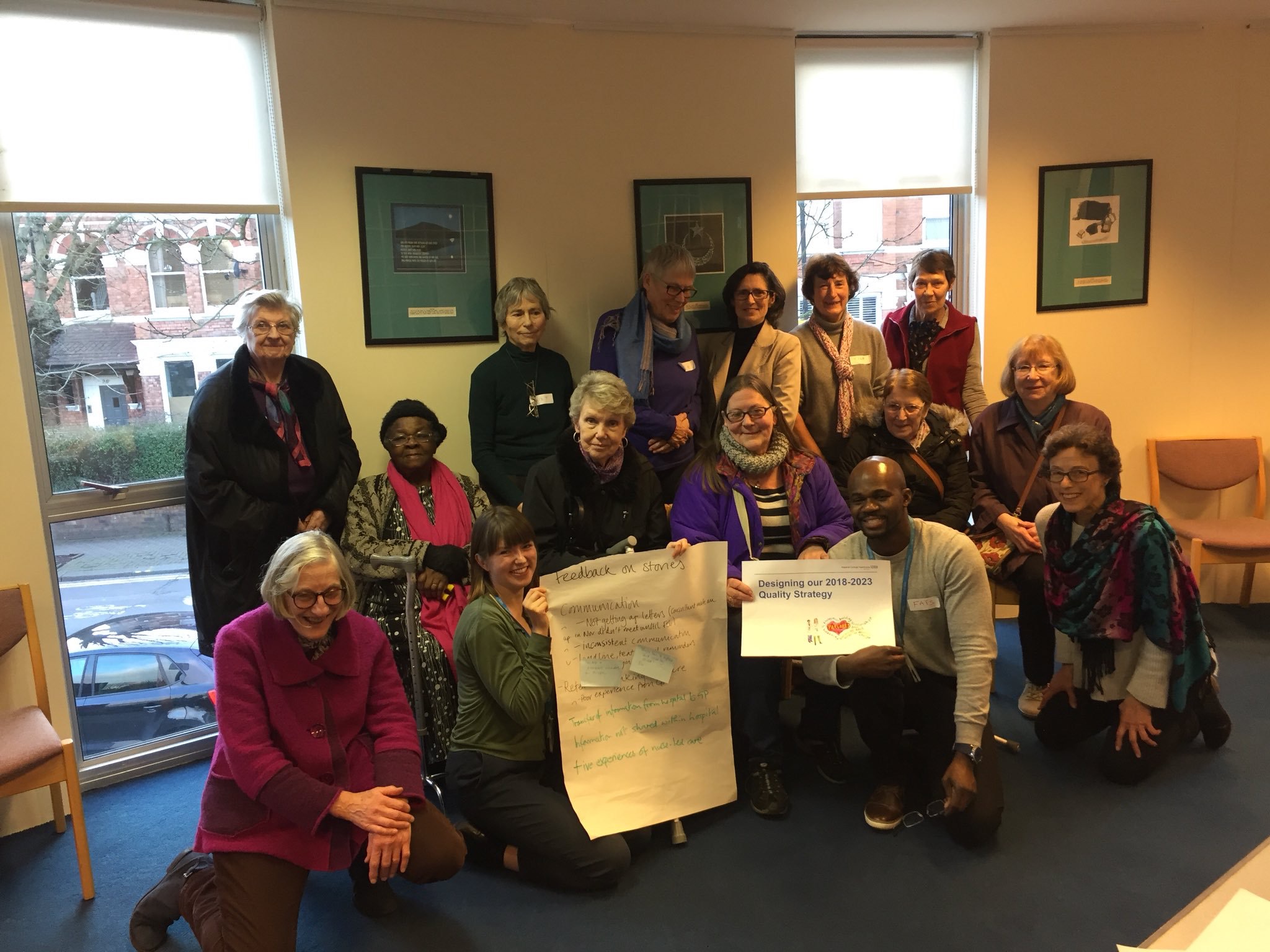
The Imperial NHS Quality Improvement team used a “community organizing approach” to run a Listening Campaign, Dec – Apr 2018. This helped them to develop their 2018-2023 Quality Strategy. Phoebe Rutherford explains how they went about it. You can hear more about their approach at their upcoming inaugural Share and Spread Improvement event.
What did you do?
We used a community organizing approach to lead a listening campaign in North West London to help shape our new Quality Strategy for 2018 – 2023. Between December and April 2018, we had around 1,000 conversations with staff, patients and community groups. In a mix of one-to-one interviews and focus groups we used a short set of open questions to define what quality means and what matters most to our patients and communities.
We carried out a thematic analysis of all the responses and used the Care Quality Commission definition of quality to organise the different themes and change ideas. We have found that there are remarkable similarities between patient and staff issues and priorities. Using the Care Quality Commission five domains of quality: safe, effective, caring responsive and well-led, we presented the key themes to help define improvement priorities for the Trust.
Who did you involve and how did you find the right people?
We partnered with Citizens UK to use community organising processes and outreach activities to reach diverse communities. A key principle for our quality strategy is inclusiveness: connecting with those who we find hardest to reach, taking steps to overcome barriers to participation and encouraging everyone to have their say. We looked at the following available data to help shape the listening campaign:
- Inpatients and outpatients admissions demographic data
- NW London population segmentation
- Translations services use (top 3 languages: Arabic, Farsi and Urdu)
- Complaints data
We had 275 one-to-one semi-structured interviews with patients at our five hospitals; St Mary’s Hospital, Western Eye Hospital, Charing Cross Hospital, Hammersmith Hospital and Queen Charlotte’s and Chelsea Hospital. We recognised that patients, carers and local people don’t ‘belong’ to one NHS organisation and that we needed to think northwest London-wide. Using community organising we spoke to 230 people from a diverse mix of local community groups, including; Newman Catholic College, London Interfaith Centre, the Al Manaar Islamic Centre, The Abbey Centre, Community Champions providers meeting, Refugee Group, Ealing Council, HM Prison Wormwood Scrubs and Westminster Mind.
What were you trying to achieve?
The listening campaign set out to re-define what quality means through the eyes of our patients, staff and community groups. We want to use the stories and experience we heard to help us to focus on what matters most to the people who use our services and strengthen the patient and public voice in the selection of annual quality improvement priorities.
Through a community organising approach, we wanted to build new alliances with community groups in northwest London and make connections with leaders in the community who are interested in co-production of health services and improving health in the community.

What impact did involving the public have on your project?
Some early outputs from our project include the involvement of women in a maternity user group supporting the improvement work at our weekly ‘Maternity Big Room’ and plans for a new volunteer group from Al-Manaar mosque to help with end of life care of Muslim patients.
“Quality for me is feeling cared for, explaining things in words I understand” (Patient). Our lay partners have helped to design and shape the listening campaign and ensure that we are using language that is easy to understand and reflects what we were told.
For involvement to be meaningful, it needs to make a difference to the lives or the experiences of service users and carers. On the 19th September we made a successful pitch to Q Community members and secured £30,000 at the annual community event from the Q Exchange to develop the community organising approach with Citizen’s UK. We want to use a formal pilot to develop relationships that will have an impact on improving the health of the communities we serve.
What was the most challenging part of doing PPI and how did you overcome it?
It has been difficult to find the time and resources to support a large-scale engagement exercise and then prioritise the change ideas against the other commitments of the improvement team. If we can maintain the networks we have built and empower citizens to lead elements of the programme it should become sustainable. We want to make involving patients, carers and local people in change ‘business as usual’ for everyone.
We have just carried out a small review of the use of patient and public involvement in quality improvement projects across the Trust to explore what barriers there are and has made a difference to projects who have used patient and public involvement. The project leads we spoke to requested a toolkit to help simplify the process, provide clarity about GDPR and provide examples of patient and public involvement across the Trust.
What do you plan to do next to do further patient and public involvement?
As well as Maternity there are 11 other clinical pathways across the Trust who hold regular ‘Big Rooms’, with support from Sheffield Teaching Hospital’s Flow Coaching Academy. Patient stories form a key part of the agenda for the Big Rooms but not all teams have managed to recruit patients to their weekly sessions to share their experiences so that is one key area to focus on.
We have just carried out a small review of the use of patient and public involvement in quality improvement projects across the Trust to explore what barriers there are and has made a difference to projects who have used patient and public involvement. The project leads we spoke to requested a toolkit to help simplify the process, provide clarity about due GDPR and provide examples of patient and public involvement across the Trust.
What advice would you give others interested in doing something like this?
Some of the successes have been down to building relationships and making use of existing networks, providing a ‘match-making’ service where we can! Specific ideas, issues and themes from the listening campaign were fed back to relevant departments and services in the organisation so that they could respond locally.
One of our first steps had been to talk to one of the cancer nurse specialists who had been doing a lot of work with community groups. Following introductory emails and we were able to book in drop in meetings with leaders from community centres and organisations across North West London.
Find out more from the team at Imperial College Healthcare NHS Trust: Hadjer Nacer @HadjerNacer, Ralph Critchley @CritchleyRalph, Sally Gimson @SallyGimson, Bob Klaber @BobKlaber, Fatai Ogunlayi @O_LaFatai and Phoebe Rutherford @PhRutherford