“No test is better than a bad test,” said Matt Hancock.
While we may tire of hearing slogans, the principle here is important.
Coronavirus antibody tests have been hailed as a game-changer for the pandemic and a way forward as we traverse these uncertain times. Antibodies are Y-shaped immune molecules produced by the body in response to an infection. They latch onto the offender – such as coronavirus – in a bid to thwart it. Your body keeps a record of the encounter, so that if it comes across the same pathogen in the future, it can quickly make more antibodies and launch an effective attack.
This is the basis for hedging bets on antibody testing for coronavirus. The idea is that the tests will flag people who have already had the infection and therefore might have protection from getting it again. And so these individuals could potentially be afforded greater flexibility than those vulnerable to the disease.
But it’s not that simple.
Despite being known for under a year, this is arguably one of the most studied viruses ever. Yet it’s still new, and there are many unknowns. Crucially, we don’t yet know whether having antibodies can prevent future infection. Or, even if they do, how long this immunity lasts – a month, a year, many years? These are all questions we must answer before a potentially dangerous over-reliance is placed on these tests.
With so many caveats, why are researchers at Imperial leading a major study of community antibody testing? While the tests’ power to indicate immunity is – as yet – far from clear, they have important uses beyond this. Rather than focussing on individuals, looking at widespread patterns at the population level could help to monitor the evolution of the epidemic, which will have important implications for easing of restrictions such as social distancing.
Antibodies vs antigens
Currently the most accurate way to look for antibodies is to perform a lab test called an ELISA, on a sample of blood. Antibodies are very selective about what they stick to – specific molecules called ‘antigens’ (in this case, bits of the coronavirus). In an ELISA, a blood sample is mixed with coronavirus antigens that are ‘glued’ onto a test surface. If antibodies are present in the sample, they stick to the antigens and this binding leads to a detectable signal, most commonly in the form of a colour change.
These lab-based tests are accurate and can tell us the exact amount of antibody in a sample, but they’re complicated to perform, and require expensive, specialised labs. This means it’s not feasible to roll out this kind of antibody testing at a national scale, when labs are already overburdened. That’s why Imperial’s REACT study is looking at the possibility of using home testing kits instead.
“The big advantage is that the home testing kits are really cheap to produce, easy to distribute and store at room temperature, and they completely bypass the lab,” says Barney Flower, Clinical Research Fellow at Imperial and member of the REACT study team. “The beauty is that you get participants to do the leg work and carry out the tests themselves, so it’s less of a capacity issue when resources are stretched.”
These home tests, called Lateral Flow Tests (LFTs), work in a similar way to ELISA, but everything is crammed into a small testing stick, which participants place a drop of blood onto. If antibodies are present, a signal will show up in a window on the testing stick, usually a coloured line.

A flooded market
By May of this year, already more than 200 of these LFTs had reached the market. However, there was no guarantee of their accuracy.
“The tests have been validated for use in laboratories, but in general their performance has been tested in small numbers of individuals, often fewer than 50 patients,” Barney says. “And these were usually individuals who were in hospital with COVID-19, so quite sick, and therefore more likely to have a strong immune response to the virus, producing lots of antibodies.”
This presents an issue, given that many people who have been infected with the coronavirus don’t have symptoms, and most don’t end up in hospital. So it’s critical to ensure that these tests work in this key group. And it’s also important to make sure that the tests perform well when they’re carried out by individuals themselves, not a trained technician – which is usually how they’re scrutinised in formal validation tests.
Antibody test results: true or false?
There are two main criteria that researchers use to assess how well an antibody test works. Its sensitivity is how well it picks up people who have been infected. If a test is 95% sensitive, for example, then out of 100 individuals who have had COVID-19, five will be wrongly identified as having not been previously infected (false negatives). Specificity, on the other hand, concerns the test’s ability to correctly identify those who were not infected. So if a test’s 99% specific, out of 100 people who haven’t had COVID-19, one will be wrongly identified as having been infected (a false positive).
In the UK, our regulator of medicines and medical devices (the MHRA), set out guidelines which stated that antibody tests need to be at least 98% sensitive to be able to guide decision-making in the clinic.
“The tests we’ve been looking at have been far below that,” Barney says. “So they’re no good at the individual level. But if we can find a test that’s really specific, we can make adjustments in our calculations and get a fairly accurate picture of the proportion of people who have antibodies at the population level.”
A testing conveyor belt
For the REACT programme, a team led by Professor Graham Cooke has been assessing a number of different commercially available tests, including the Wondfo test that the UK Government stockpiled early on in the epidemic. In the first phase, researchers carried out a small-scale study to test accuracy and usability (how well people can perform the test by themselves) on a group of around 270 healthy people, all NHS staff. Importantly, they’d all had a previous diagnosis of COVID-19 confirmed by a nose swab, but none of them had been hospitalised from the disease.
“The first test we tried out was throwing out negative results in four out of five participants – in a group who’d all had confirmed infection,” Barney says.
As well as testing the positive cases’ blood with the antibody kits, the researchers also performed an accurate lab ELISA to check if antibodies were detectable on the best test available. They found antibodies were present in more than 95% of cases.
They also tested the antibody kits on a batch of 500 blood samples taken from 2019 or earlier, i.e. preceding the pandemic and therefore COVID-19-free.
Together, this process is allowing the researchers to determine the tests’ sensitivity and specificity with a high degree of confidence.
“We’ve now developed a system where we can continually bring in new tests as they emerge, evaluate them on our bank of ‘known positive’ and ‘known negative’ samples, and if they look good we can test them in the clinic in more of a real-life scenario,” Barney says. “It’s like a lateral flow test conveyor belt.”
It’s how you use it
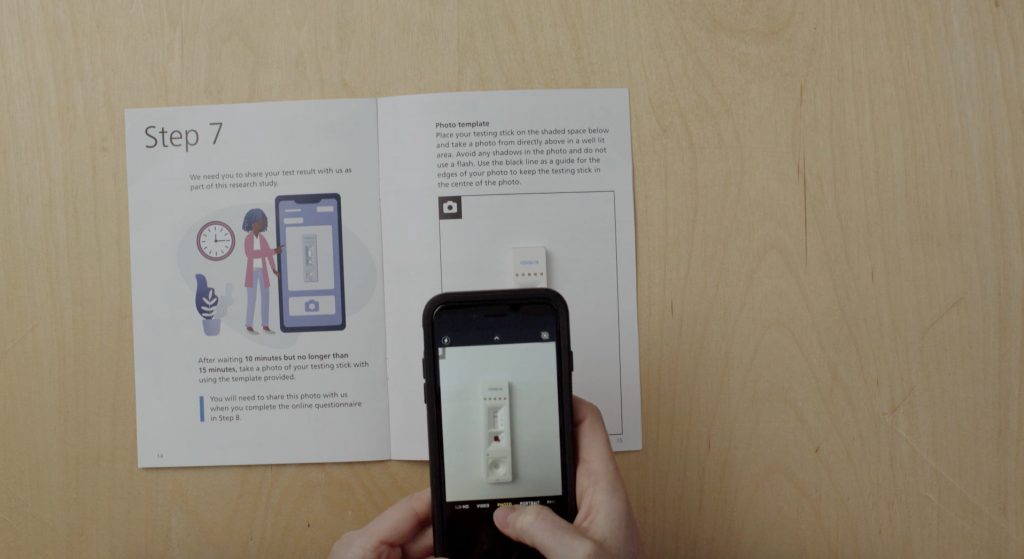
Another vital aspect of this work has been determining how usable these tests are by members of the public. Even if they perform well in controlled environments, they’re no good for use en masse if people can’t do them at home. A huge effort has been underway at Imperial, led by Prof Helen Ward, to involve and engage the public in this part of the project. Thousands of volunteers to date have given their time, offering valuable insight that’s not possible to gauge through lab testing alone.
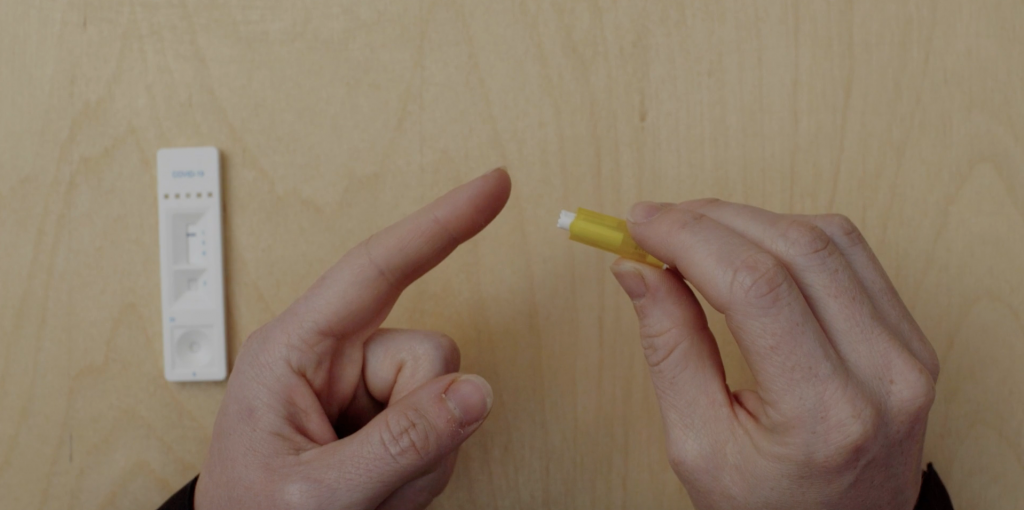
While all of the LFTs work in the same way – placing a drop of blood onto a testing stick – there have been a number of issues with usability that this public involvement exercise has flagged up.
“This has been so important to highlight real issues with the tests,” Barney says. “One of the major things has been getting enough blood from the finger-prick, and successfully dropping this on the right part of the testing strip.”
At the start of the study, participants were provided with a plastic pipette to collect their blood after pricking their finger, which was then used to transfer a droplet of their blood onto the stick. But this soon proved a fiddly procedure, and now individuals are asked to place a drop of blood directly onto the test.
“We also found that health professionals tended to dive straight in and pay less attention to the instruction manual, and were therefore more likely to get it wrong!” Barney recounts. “Clear, simple instructions are so important!”

Blood, spit, spots
While this research continues, the REACT team has narrowed down their hunt for the best home LFT. After analysing 11 different LFTs in the lab, they found the best tests could correctly identify individuals with coronavirus antibodies over 80% of the time, while also correctly ruling out those who don’t in more than 98% of tested individuals.
Based on these findings, the team selected and rolled out a finger-prick test to more than 100,000 people across England, who tested themselves at home in June and July. Covering all 315 local authorities to ensure a nationally-representative sample, this major study found that just under 6% of the population had antibodies to coronavirus and had therefore likely already had COVID-19. It also revealed that the virus hadn’t spread evenly across the country, disproportionally affecting key workers and Black, Asian and minority ethnic individuals.
Watch the video below for the study highlights:
Today we announced our findings of the world’s largest study on home coronavirus antibody testing. @imperialcollege researchers show that around 3.4 million people in England may have already had #COVID19, but that it hasn’t spread evenly across the country.
Find out more 👇 pic.twitter.com/JvUOxv9mdl
— Institute of Global Health Innovation (@Imperial_IGHI) August 13, 2020
https://platform.twitter.com/widgets.js
The team is continuing further testing of LFTs on a group of 5,000 key workers to gather more data. This particular piece of work is also investigating whether other methods could also be used for antibody testing, such as saliva samples or drops of blood dried on paper.
While this research can’t tell us anything about possible immunity levels, its offering is a greater understanding of how the epidemic is progressing, and who is at greatest risk from the infection.
“What this can help us understand is how many people have been exposed to the virus,” Barney says.
“Comparing these numbers to deaths and numbers admitted to hospital, in different populations and different parts of the country, will help plan for future outbreaks.
“However, it’s still important to say that we don’t know what these antibodies mean for individuals yet. Do they offer protection? And if so, for how long? The future of mass antibody testing rests on what we can learn from research like this.”
If you’d like to learn more about the REACT studies, visit our website here.