The majority of people who die every year would prefer to die at home, yet only about half achieve this.
This is often due to not being able to manage symptoms at the end of life. People often have to wait longer than what feels acceptable to them for district nurses to come and administer injections. When this happens, symptoms can escalate, carers and patients can become distressed and families lose control of the situation.
Such poor management of pain relief at the end of life can lead to unplanned emergency admissions, resulting in poorer quality of life and poorer experiences for carer and patient. Laycarers care for their loved ones’ physical and emotional needs and when faced with suffering, many want to do more, including clinical tasks, with the support of healthcare teams.
We believe there should be a choice for carers to be trained to give symptom control medications. It’s important to note, though, that this is not an expectation, and carers must be deemed suitable by healthcare professionals.
Yet there is no single national policy to do this, and different regions have different policies. For example, Lincolnshire developed a policy in 2013 to support a very rural population that was experiencing frequent delays in getting to patients due to distance and remoteness.
In addition, the majority of the policies that do exist are mostly used by carers who are also healthcare professionals. And historically, educational tools to support policies are poor and rely upon literacy being high, despite the average reading age in the UK being nine years old.
Supporting carers to administer medication at the end of life
In 2019, the CARiAD Feasibility Study in Wales set out to determine if carer-administration of as-needed subcutaneous (under the skin) medication for specific symptoms, including pain, in home-based dying patients would be feasible and acceptable in the UK. It found that waiting times of patients to receive sub-cut injections from District Nurses compared with carers in Wales went from 105 minutes to 5 minutes.
Carers reported that they were “at first nervous, but then felt confident. It gave me comfort knowing that I could help mum’s symptoms. I enjoyed helping with mum’s care” and that they “…thought it was an excellent experience and such a help and comfort in knowing I could administer medication to help my relative and not have to wait for a HCP to arrive”.
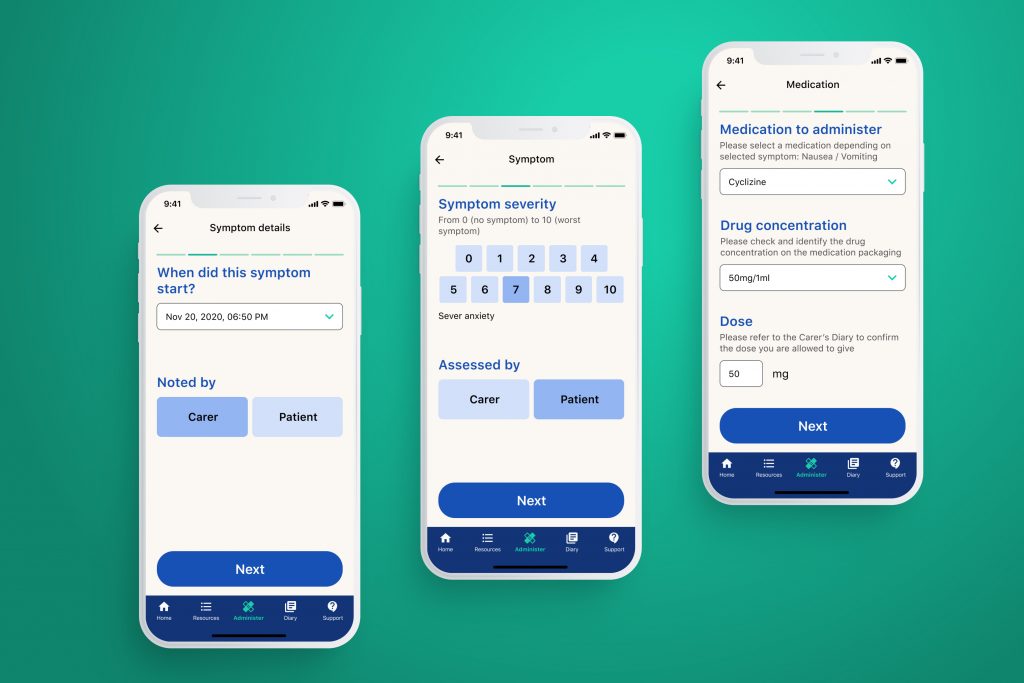
We are now working with the CARiAD team, along with NHS and hospice partners, to develop a technology-driven support tool for carers. We aim to reduce friction in the experience to administer medications, improve the confidence levels of carers, improve the overall experience of managing symptoms and treatment in the home, and unlock opportunities for robust data collection for quality improvement and improved patient safety.
Palliate, a digital support app for carers
Our solution, Palliate, seeks to improve the access and quality of training and support for carers to administer sub-cut medications in the home, to support patient preferences for a home death while also reducing pressure on community care teams. It does this by providing digital information and support via an app, to carers who have been trained to deliver medications.
In March 2020, we accelerated the development of Palliate in response to COVID-19. The virus is re-writing the way in which end-of-life care is done in the community: district nurses and nurse specialists were denied access to patient homes, resulting in more families needing to more themselves, in an uncertain environment.
In response, the Helix Centre rapidly deployed a website tool that incorporated the training materials and processes, that was used by NHS and hospices teams during the first wave.
Through that we were able to swiftly validate the role of design and technology to support community palliative care, especially in a crisis, and our learnings are helping to improve Palliate as we continue its development.
Ivor Williams is a Senior Design Associate at IGHI’s Helix Centre. His other projects including developing innovative technology-based solutions to improve children’s hospice care.