Living with Type 2 Diabetes (T2D) can feel like a full-time job. Regular check-ups, monitoring blood sugar levels, adjusting medications, and managing lifestyle changes all demand time and effort. For the 460 million people worldwide dealing with diabetes (a number projected to climb to 700 million by 2045), finding convenient and effective healthcare solutions is more critical than ever. Enter virtual consultations (VC); a modern approach to healthcare delivery that is transforming how people with T2D manage their condition. Our recent systematic review and meta-analysis published in the Journal of Diabetes Science and Technology sheds light on just how powerful this tool can be. Let’s examine the benefits of virtual consultations for people with T2D and why they’re becoming more important in the care of people with long-term conditions like T2D.
Convenience Without Compromise: Effectiveness Matches In-Person Care
One of the key findings from the review is that virtual consultations are just as effective as traditional face-to-face visits when it comes to managing T2D. The meta-analysis, which included 15 studies and over 821,000 participants, showed no significant difference in HbA1c reduction (a key marker of blood sugar control in people with T2D) between virtual and in-person care. Whether it’s monitoring blood pressure, lipid profiles, or glycaemic levels, VCs hold their own. This means you can get appropriate care from the comfort of your home without sacrificing results. For busy people juggling work, family, or mobility challenges, this is very positive news – good quality care no longer always requires a trip to the clinic.
Saving Time and Money: Efficiency at Its Best
Time is money, and virtual consultations save both. The review highlighted how VCs cut down on the need for frequent in-person visits, reducing travel time and costs. One study found that treatment costs dropped by an average of $135 per patient with VCs—a significant saving for both individuals and healthcare systems. Another showed that while face-to-face care often required visits every one to two weeks, virtual care patients needed only one or two appointments over four months. VCs make diabetes management more efficient, freeing up time for what matters most.
Care When You Need It: Timeliness That Counts
When it comes to long-term conditions like T2D, timely adjustments to treatment can make all the difference. Virtual consultations have a role here as well. The review noted that the average time to an initial visit dropped from 106 days to just 46 days after implementing VCs. Faster access to healthcare providers means quicker feedback, medication adjustments, and support, helping keep your condition in check. Patients also reported shorter wait times and more flexible scheduling, making it easier to fit care into busy lives.
A Personal Touch: Boosting Patient Satisfaction
You might think remote care feels impersonal, but the data says otherwise. The review found high levels of patient satisfaction with VCs, with 83% of participants in one study rating them as helpful and convenient. Another 76% felt that tools like FaceTime made their care more interactive and engaging. Patients especially appreciated the flexibility of VCs during the Covid-19 pandemic, and many expressed a desire to stick with virtual care long-term. It’s not just about convenience. It is also about feeling heard and supported in a way that fits your lifestyle.
Bridging Gaps: Improved Access for Some
For people in rural areas or those with mobility issues, getting to a clinic can be a hurdle. Virtual consultations break down those barriers. The review pointed out that VCs can increase access to care, particularly for rural patients or those who struggle with transportation. One study even noted higher rates of preventive measures – like statin prescriptions – with VCs, suggesting that remote care can enhance certain aspects of diabetes management. While there is still work to be done to ensure everyone benefits equally (more on that later), VCs are a step toward making healthcare more accessible.
A Few Caveats: Safety and Equity Challenges
No solution is perfect, and the review flagged some areas to watch. Safety-wise, VCs can not fully replace physical examinations – such as checking for foot ulcers or neuropathy – which could miss some issues if VCs are not paired with in-person visits. On the equity front, younger, patients tend to thrive with VCs, showing greater HbA1c improvements and higher satisfaction. Older adults or those with lower digital literacy, however, faced challenges like technical difficulties or lower comfort with the technology, leading to less impressive outcomes. The digital divide is real, but it’s not insurmountable. But policies to boost digital literacy and access are essential.
Conclusions
Virtual consultations aren’t just a stopgap. They are a viable, long-term option for managing people with Type 2 Diabetes. They match in-person care in effectiveness, save time and money, deliver timely support, and keep patients happy. While there is room to improve safety and ensure everyone can benefit, the potential is clear. As the review suggests, integrating VCs into routine care, paired with efforts to bridge the digital divide, could improve how we support people with T2D to manage their condition.
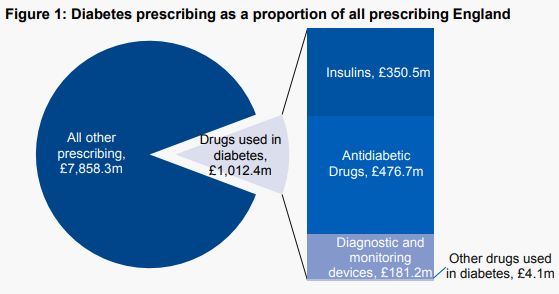 Drugs used to treat diabetes are now responsible for 11.4% of total primary care prescribing costs in England, £1,012 million annually. The very high costs to the NHS of treating diabetes are an inevitable consequence of the increase in the prevalence of type 2 diabetes in recent decades. This increase in the prevalence of type 2 diabetes is in turn a consequence of lifestyle factors such as high-calorie diets (particularly diets high in sugars and refined carbohydrates), physical inactivity and obesity. We need effective strategies at both population and individual level, and changes in the obesogenic environment we live in, to reverse these adverse lifestyle- associated factors and bring down the prevalence of type 2 diabetes.
Drugs used to treat diabetes are now responsible for 11.4% of total primary care prescribing costs in England, £1,012 million annually. The very high costs to the NHS of treating diabetes are an inevitable consequence of the increase in the prevalence of type 2 diabetes in recent decades. This increase in the prevalence of type 2 diabetes is in turn a consequence of lifestyle factors such as high-calorie diets (particularly diets high in sugars and refined carbohydrates), physical inactivity and obesity. We need effective strategies at both population and individual level, and changes in the obesogenic environment we live in, to reverse these adverse lifestyle- associated factors and bring down the prevalence of type 2 diabetes.