Of all the covid-19 vaccines currently licensed or in development, the Oxford-AstraZeneca vaccine was considered the vaccination of choice by many countries because of its low cost and ease of storage compared to other vaccines. In the UK, more than 25 million people have had their first dose of covid-19 vaccine, comprising almost half of the adult population, with either the Oxford-AstraZeneca or Pfizer-BioNTech vaccines.
The UK Medicines and Healthcare products Regulatory Agency (MHRA) has monitored the safety of both vaccines through the Yellow Card scheme—a mechanism of reporting any possible vaccine side effects known as adverse drug reactions (ADRs). However, these reports do not mean there is causal link between the use of a vaccine and side effects. Data up to 7 March shows an estimated 11.7 million first doses of Oxford-AstraZeneca and 10.9 million doses of Pfizer-BioNTech vaccines were administered in the UK, resulting in 35,325 and 61,304 reports of possible side effects for Pfizer and AstraZeneca vaccines respectively, indicating a very low rate of reported side effects. The overwhelming majority of reports consist of injection-site reactions and symptoms secondary to the normal immune response such as “flu-like” illness, headaches, chills, and fatigue. All these are in line with the findings from clinical trials and from side effects reported with other routinely used vaccines.
Reports of severe allergic reactions to the Pfizer (223 reports) and AstraZeneca (234 reports) vaccines have been very rare. Available MHRA data do not suggest that venous thromboembolism is caused by the AstraZeneca vaccine. To date, there have been five reports of cerebral venous sinus thrombosis to MHRA, a rare type of blood clot in the cerebral veins, with no causal association with the vaccine. The temporal association between vaccination and death in mostly elderly patients with health conditions have also been reported in about 500 cases. However, there is no evidence to support that vaccination caused these deaths.
While the investigations of a potential link between AstraZeneca vaccine and thromboembolic events continue, the MHRA, the World Health Organization (WHO) and the European Medicines Agency (EMA) have ruled out the causal link and stated that the population benefits far outweigh the risks, thereby reaffirming the safety of the vaccine that over 17 million people in the UK and EU have so far received. Around 30 cases of thromboembolic events have been reported amongst five million vaccinated people in EU; this rate remains lower than that observed in the general population.
Receiving a covid-19 vaccine is a landmark and memorable event for people and this coupled with a heightened sense of awareness following vaccination may lead to more cases being picked up. Moreover, there will be more presentations and over-diagnoses of thromboembolic events as expected following a highly publicised safety scare such as this.
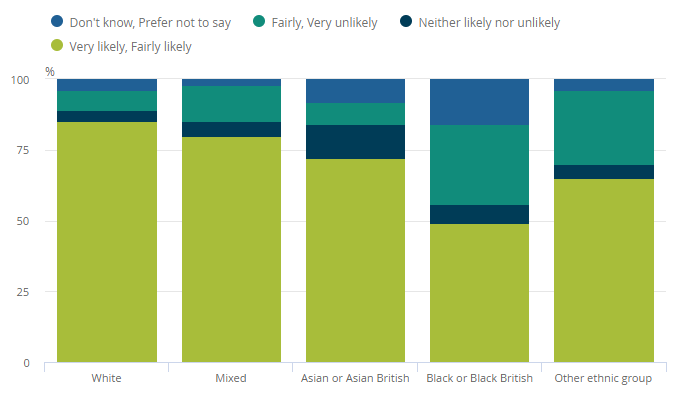
While routine monitoring of vaccines to avoid potential harms is necessary, pausing or delaying vaccines must be evidence-based. The speculative commentary, generated by the media, will have serious and unintended consequences including an increase in vaccine hesitancy and even refusal; across Ireland, 30,000 vaccination appointments were cancelled during the week starting 15 March. Safety signals occur often with vaccines, with the majority representing false signals; although well-intentioned, the misapplied precautionary principle will undermine public trust, and heighten covid-19 risk through amplification of misinformation and disinformation campaigns of the “anti-vaxxer” movement. Vaccine-hesitant individuals are concerned about side effects and health-related long-term effects; these reports will make it very challenging to overcome these concerns at a time when covid-19 cases are still increasing across many European countries, requiring optimal uptake of vaccines to limit the impact of the covid-19 pandemic on populations.
The risks and trade-offs of suspending a life-saving vaccine must be carefully weighed especially during a pandemic; covid-19 itself is associated with blood clotting disorders. Historical precedents show that widely publicised safety scares have profound and long-lasting influence on vaccine confidence. [1] In 2017, the announcement that the dengue vaccine, Denvaxia, posed a risk to those who had not previously been exposed to the virus caused a drop in vaccine confidence in the Philippines and Indonesia. The safety controversy around the human papillomavirus vaccine in Japan caused one of the sharpest declines in vaccine uptake (from approximately 74% in those born in 1994-1998 to approximately 0.6% for those born in 2000). [2] The shock of this still reverberating today with Japan ranking among the lowest in vaccine confidence in a worldwide study. [1] A decline in vaccine uptake was also observed in Indonesia following warnings by the country’s faith leaders. [3]
Covid-19 vaccines are the single most effective way to prevent severe illness and death from the disease and accelerate the re-opening of society following non-pharmacological interventions such as lockdowns. Furthermore, vaccines are safe and have contributed to saving millions of lives. We call for monitoring of vaccine safety to occur out of the media limelight as sensationalist and exaggerated reporting will do irreparable damage to vaccine confidence. This includes suggestions by some media outlets that the actions taken by European countries were driven by political reasons. Sensationalist media reporting will lead to increased vaccine hesitancy, further loss of lives and derail efforts to end the current pandemic. Governments responses must be led by independent evidence through established public health and regulatory bodies such as the WHO, EMA and MHRA.
Mohammad S Razai, Academic Clinical Fellow in Primary Care, St George’s University of London.
Tasnime Osama, Honorary Clinical Research Fellow, Department of Primary Care & Public Health, Imperial College London.
Azeem Majeed, Professor of Primary Care & Public Health, Department of Primary Care & Public Health, Imperial College London.
This article was first published on BMJ Opinion