“The potential that my research could lead to the understanding of how bacteria cause disease and potentially the identification of drug targets that can impact people’s infections is really motivating.”
Cystic fibrosis is a life-limiting genetic condition that causes the body to produce thick, sticky mucus, primarily affecting the lungs and digestive system. Over 11,000 people in the UK are living with the condition.
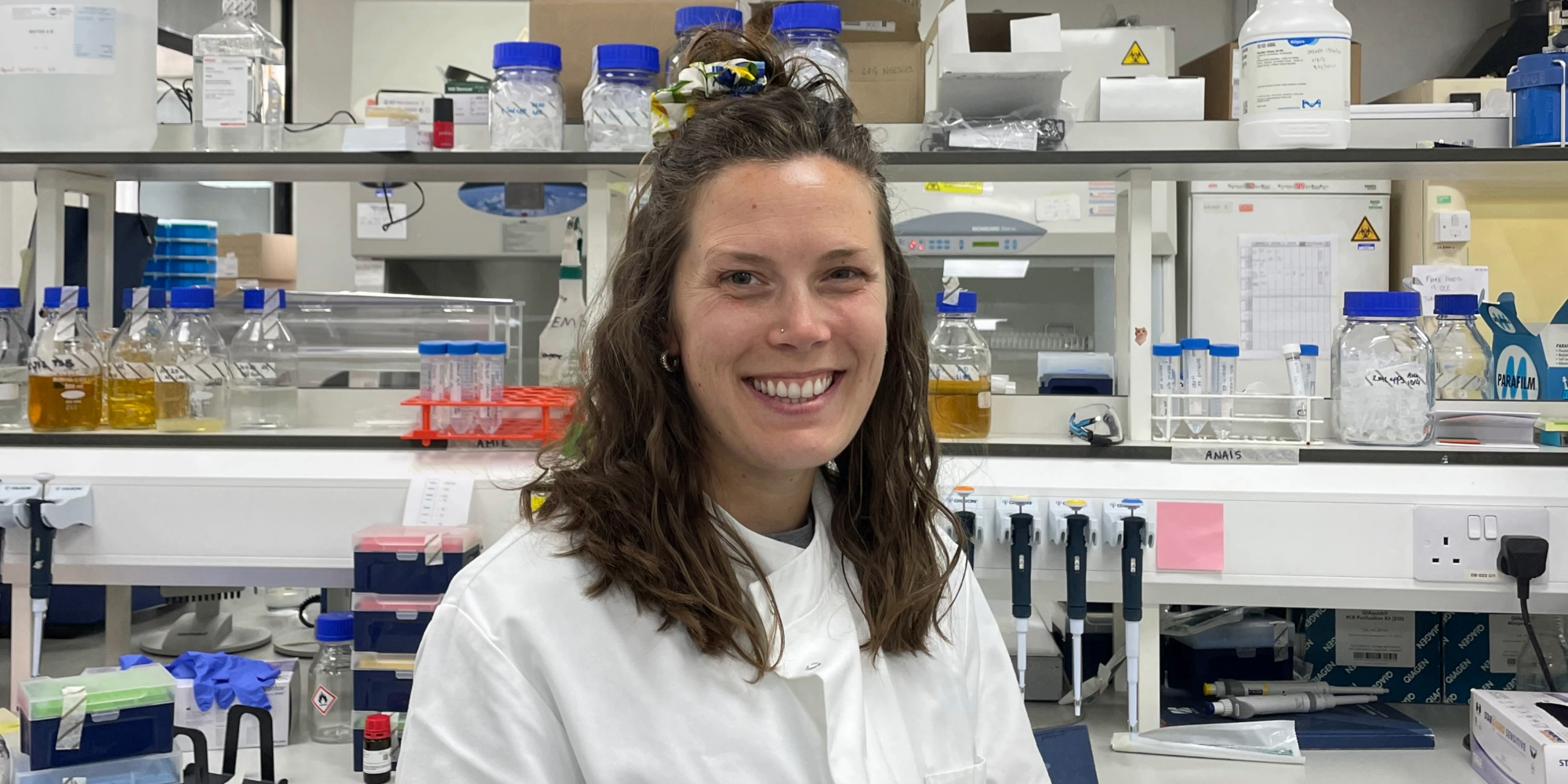
As part of Cystic Fibrosis Awareness Week (9–15 June 2025), we spoke with Harriet Ellis, a Research Associate in the Allsopp Group, whose work focuses on understanding how Pseudomonas aeruginosa – a key bacterial threat to people with CF – adapts and causes infection. She shares how her research could one day help prevent serious lung infections and why cross-disciplinary collaboration is essential to driving innovation in cystic fibrosis research.
What is your current research into cystic fibrosis focusing on?
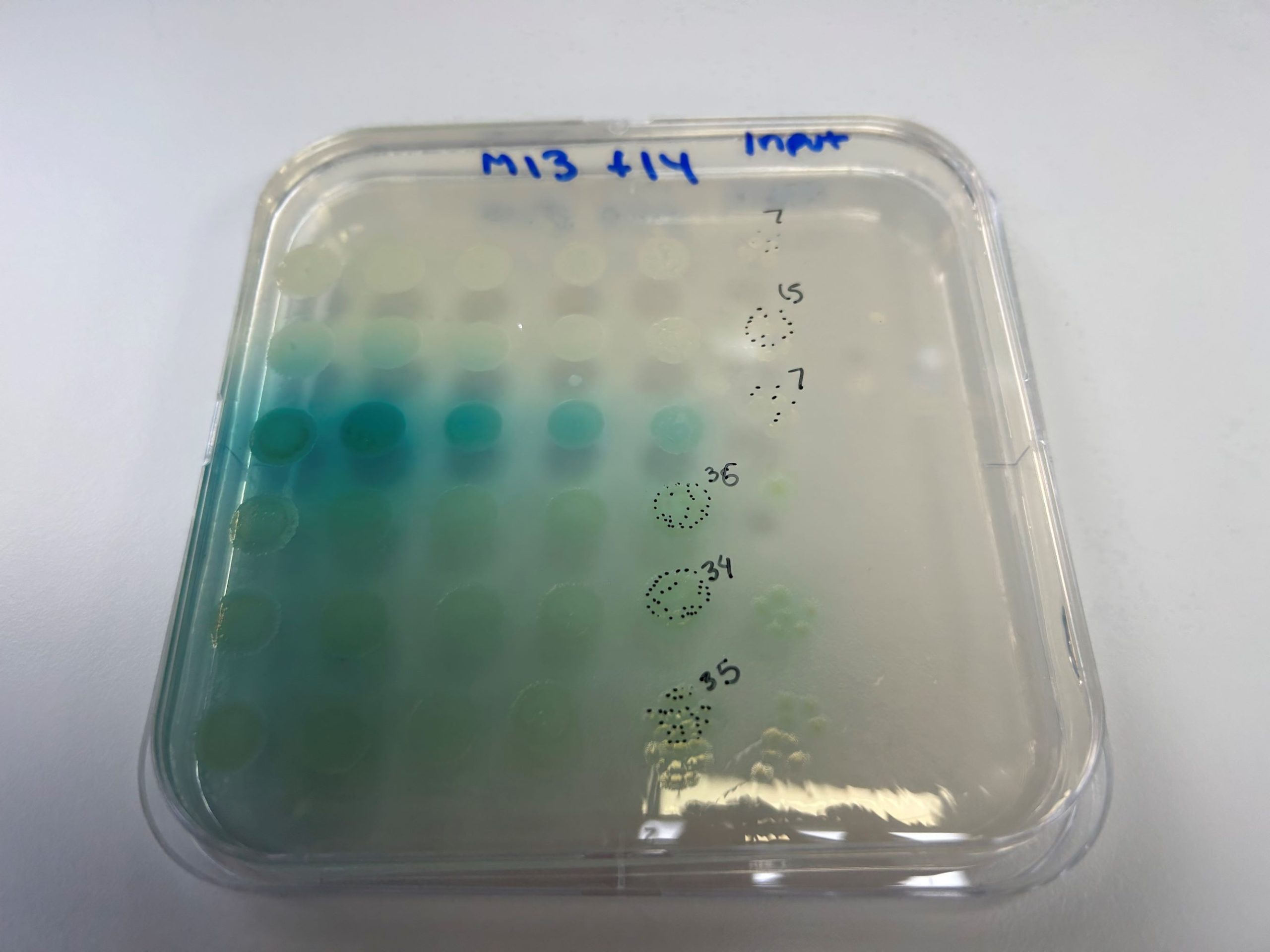
My research focuses on the bacteria Pseudomonas aeruginosa, which is one of the most common bacteria infecting the lungs of people with cystic fibrosis (CF). CF is an autosomal recessive gene disorder with a global burden of approximately 162,400 people worldwide. Due to an impaired immune function and defective clearance, some bacteria, such as P. aeruginosa can colonise the lungs, which leads to worse patient outcomes. Pa is also on the WHO critical list of pathogens to investigate, as it develops resistance to a lot of treatments and causes lots of problems in hospitals. My project in the Allsopp Group specifically looks at how P. aeruginosa responds to its environment to switch on protein machines that help it adapt to different environments, damage human cells, and compete with other bacteria. I want to figure out how these protein machines are controlled by the bacterium!
What impact do you hope your research will have?
My research is fundamental and will contribute to the understanding of how bacteria colonise people and which proteins they use to do it. If we know this, we can then try to develop strategies or drugs to block these bacterial proteins or switch them off. The potential that my research could lead to the understanding of how bacteria cause disease and potentially the identification of drug targets that can impact people’s infections is really motivating.
What does a typical day look like for you?
It always starts with a cup of coffee and reviewing my daily schedule. Lab experiments are a lot like cooking; everything has to be done at a specific time, so the more preparation, the better. I like to get my experiments started early, and during breaks, I’ll work on reading papers related to my research or getting my admin done.
Collaboration is key in scientific research. Have you had the opportunity to collaborate with other researchers or organisations in the cystic fibrosis field? If so, who has inspired you, or what have you learned from those partnerships?
We have a very collaborative research environment and are actively encouraged to get involved with related research projects. In the last year, I have contributed to a research project that is led by a French group and a collaborative project with clinicians in Professor Jane Davies’ group. I’ve really enjoyed these projects as I’ve gotten to work not only with other scientists but also clinicians, who have a completely different perspective on research.
What are the next steps in your research, and what advancements do you hope to see in cystic fibrosis research in the next 5 to 10 years?
I would like to see advancements in preventing severe bacterial infections in people with CF. Hopefully, my research determining how these bacteria control their changes in behaviour during the infection process will contribute to new research into combating these pathogens.
If you could see one significant change in the cystic fibrosis field within your lifetime, what would it be?
A way to remove the pathogens and restore the commensal ‘good guy’ lung microbes would be a big step forward in the field that could have a huge impact on how people with CF live.
Find out more about our Respiratory Infections research at NHLI and show your support by wearing yellow on the brightest fundraising day of the year, Friday 13 June.