“There is a growing recognition that healthcare needs to move beyond the clinic and into people’s everyday lives.”

It’s currently Know Your Numbers Week, an annual campaign led by Blood Pressure UK to raise awareness of high blood pressure and the importance of regular checks. A year on from his previous blog, How home monitoring is redefining hypertension care, we catch up with Dr Amit Kaura as he shares updates on the ongoing challenge of hypertension, including new developments in NHS care pathways designed to better support patients both digitally and non-digitally.
Written by Dr Amit Kaura, Honorary Clinical Lecturer, National Heart and Lung Institute.
The Ongoing Challenge of High Blood Pressure
High blood pressure, also known as hypertension, affects over one in four adults in the United Kingdom. It remains one of the leading causes of heart attacks, strokes, kidney disease, and other serious illnesses. The condition often has no symptoms, meaning many people are unaware they have it until serious damage has already occurred. Even after diagnosis, long waits between appointments and limited support in daily life can make it difficult to manage effectively.
Rethinking How We Support People with Hypertension
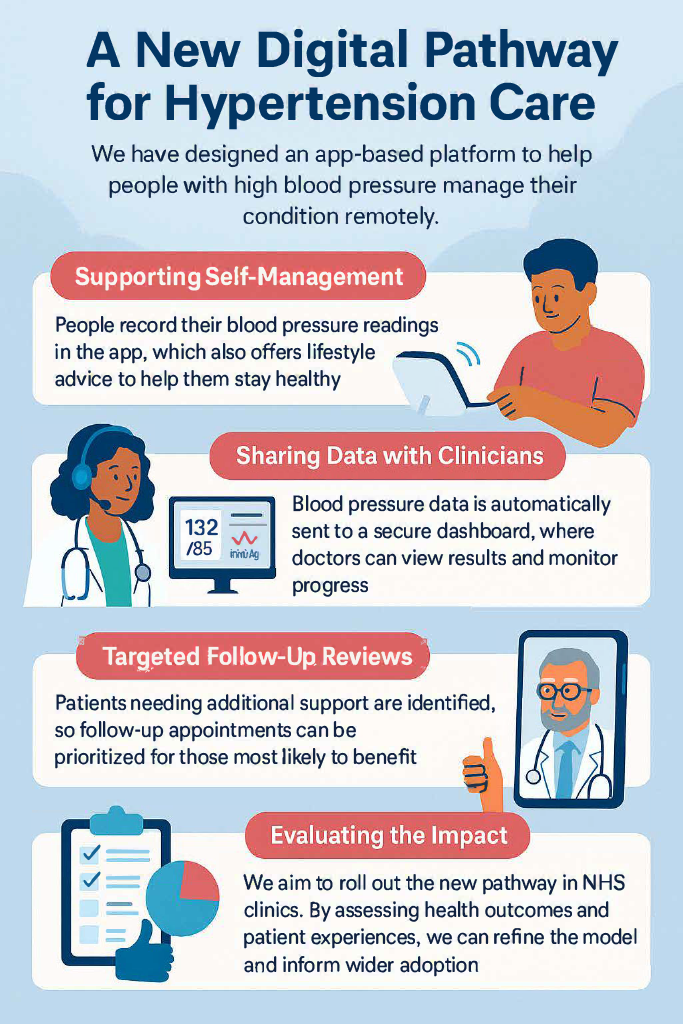
Over the past year, we have worked with NHS clinicians, digital health teams, and patients to design a new care pathway for people referred to hospital hypertension clinics. The aim was simple: to provide more responsive and personalised support that extends beyond the traditional clinic appointment.
At the heart of the new pathway is the idea that managing blood pressure is not just something that happens during a visit to the doctor. It is a daily effort that depends on a person’s routines, understanding, and confidence. The new pathway was developed to reflect that reality and to help people stay engaged and supported between appointments.
A New Digital Option for NHS Care
The service includes a digital platform that people can use at home. Patients are invited to register as soon as they are referred to the specialist clinic, which means they can begin recording home blood pressure readings and accessing personalised lifestyle support right away.
The app helps people track their progress, learn about their condition, and receive reminders to take prescribed medications. It also supports healthy behaviours such as changes in diet, physical activity, sleep, and stress management. This gives people more control over their own care and encourages regular monitoring in a way that is both accessible and easy to maintain. Clinicians can also view this information securely, which allows for more informed and timely decisions.
A Non-Digital Option for Inclusive Care
Not everyone wants or is able to use digital tools. That is why the new model includes a non-digital version of the service. This provides similar support through printed materials, phone check-ins, and in-person care. Everyone receives the same level of clinical input, and the choice between digital and non-digital formats ensures that care is fair and accessible to all.
Designed with the NHS in Mind
This new pathway builds on existing NHS processes and systems. It does not replace clinical care but enhances it by filling the gaps between appointments. During the design process, we assessed a range of platforms using a structured scoring system. We considered factors such as safety, ease of use, and how well each platform could connect with NHS systems. The chosen platform has already been used in other NHS programmes and meets national standards for data security and integration.
What Comes Next?
In the coming year, we aim to roll out the new pathway in several NHS clinics to test how well it works in practice. This is ]a real-world evaluation of a new way of delivering care. We will be looking at how the service supports patient engagement, improves blood pressure control, and fits within the usual NHS workflow.
We will compare outcomes from people using the digital platform with those receiving standard care. This will help us understand the strengths of the new model and identify any areas for improvement. Our hope is that the findings will guide future decisions about how hypertension services are delivered more widely.
Looking Ahead
There is a growing recognition that healthcare needs to move beyond the clinic and into people’s everyday lives. Better blood pressure control can prevent serious illness, reduce hospital admissions, and help people live longer and healthier lives. By making support more personal, practical, and proactive, we believe this new model can make a real difference.
As we move into the next phase of this work, we remain committed to sharing our learning and working with partners across the NHS to build services that truly meet the needs of people with high blood pressure.