Cancer survival is improving and today, half of people diagnosed will survive their disease. This is thanks to research. Research that’s guiding governments to change their policies, underpinning awareness campaigns and educational initiatives, turning discoveries into treatments and prevention measures.
But there’s still much to be done to help more people survive, by catching the disease earlier and developing better treatments.
This World Cancer Day, and as part of our celebrations to mark IGHI’s 10th anniversary this year, find out how our researchers are working to make that happen. Join us in exploring some of our projects that could lead to better detection, diagnosis and treatment of cancer.
Using AI to help spot breast cancer
We’re helping to prove the potential for artificial intelligence to improve breast screening.

IGHI is part of a collaboration – including DeepMind and Google Health – which is training computers to identify tumours in mammograms using a technique called machine learning. The team’s recent study, published in Nature, found that their AI system was as good as doctors at picking up cancers – and in some cases even outperformed them.
Breast screening involves taking x-ray images, or mammograms, of breast tissue which are then analysed by human experts. While screening continues to help save lives by picking up cancers earlier, sometimes tumours are missed. It can also lead to unnecessary treatment for tumours that wouldn’t have gone on to do any harm. That’s why our researchers are examining whether artificial intelligence could reduce the rate of error in the analysis of breast screening, and ultimately improve the management of breast cancer.
“We hope this work could minimise the burden of breast cancer in the UK and internationally,” says Mr Hutan Ashrafian, study author and IGHI scientific advisor. “Not only that, but we also believe this system has the ability to support clinicians by freeing up resources and allowing them to spend more time with patients.”
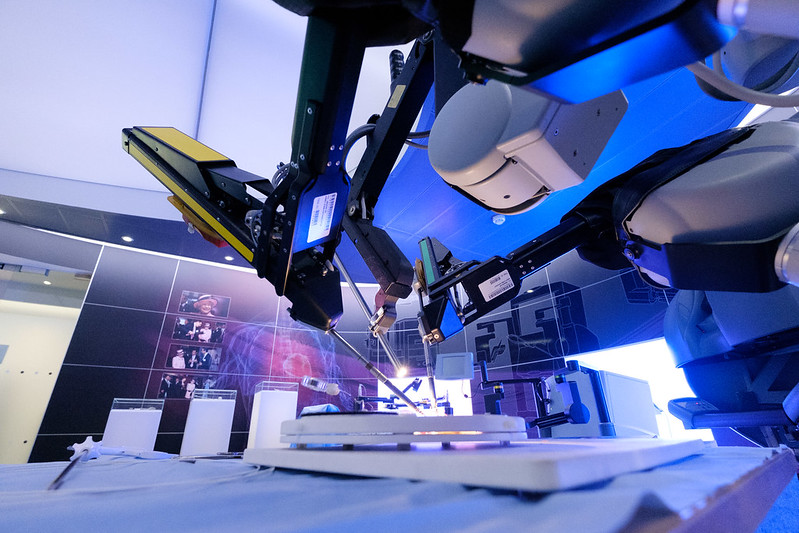
Robots for safer brain tumour surgery
Our researchers are working to make brain tumour treatment more precise, with the assistance of a bespoke intelligent robotic platform.
Researchers led by Dr Stamatia Giannarou from our Hamlyn Centre are integrating a number of imaging techniques and robotic instruments to develop a system that can more accurately characterise brain tumour tissue, and distinguish this from surrounding healthy tissue. In doing so, not only could the platform enable more accurate diagnosis, but it could also guide treatment decisions and help surgeons remove more of the cancerous tissue.
Brain tumours are very difficult to treat and survival remains stubbornly low. Surgery is the mainstay of treatment for many brain tumours, but being surrounded by delicate tissue makes the procedure particularly problematic. Surgeons can’t afford to remove too much tissue or risk serious side effects, yet remove too little and the treatment will be ineffective. Giannarou’s system hopes to change this.
“I’m passionate about contributing to a highly challenging research area, where we need significant advances in robotic vision to be able to navigate challenging and dynamic environments like the brain,” she says.
Supporting decision-making for suspect cancer
We’re launching a new project to guide the development of tools that are designed to support GPs’ decisions when managing patients with suspect cancer.
Cancer risk tools are algorithms that combine certain risk factors – like age and smoking status – with tell-tale symptoms to work out the probability of a person being diagnosed with cancer within a specific timeframe. Many patients present with symptoms that could indicate cancer, so these tools assist GPs in their decisions on who to investigate and refer.
Dr Olga Kostopoulou, research lead from our NIHR Patient Safety Translational Research Centre, will be investigating how these algorithms interact with GPs’ clinical judgment. She’ll be assessing things such as user trust and control, and looking at other concerns from GPs which could influence their decisions for urgent referral.
“The project aims to provide empirical evidence on these issues,” says Dr Kostopoulou. “And, in doing so, contribute to the currently expanding knowledge base about how such tools should be designed and introduced in clinical practice.”
Imaging to detect and track advanced disease
IGHI researchers are developing an imaging tool that they hope could detect or diagnose changes in cancer that has spread, or metastasised.
Endoscopies are a commonly used investigative technique, which traditionally relies on white light to image tissue inside the body. Prof Dan Elson from our Hamlyn Centre is testing out a different type of endoscopic imaging, called Polarization- and Multispectral-resolved Endoscopy. This uses different properties and wavelengths of light to reveal more information about tissues than is possible with traditional techniques, which can essentially only capture what the naked eye can see.
Prof Elson is investigating whether this type of imaging could help detect and characterise metastases in the tissue that lines the abdomen (peritoneum). For this work, they’re collaborating with the PIPAC trial that’s testing out a new treatment for advanced bowel cancer.
“The PIPAC trial is a good setting for us because the team regularly performs biopsies which we can image in the operating theatre,” says Prof Elson. “We also have the opportunity to image in vivo at different phases of treatment, potentially in the same patient.” Ultimately, doing so could help guide decisions in the clinic.
Making tissues glow to improve breast cancer surgery
Scientists at our Hamlyn Centre are developing an imaging system based on fluorescence that could help guide breast-conserving surgery. 
They’re using a fluorescent dye that could help highlight differences between healthy and cancerous tissue, and a special camera system that can image these characteristics. The researchers hope this work could make the treatment more accurate by enabling surgeons to see tumours during surgery, reducing the likelihood of cancerous tissue being left behind.
“By making it easy for the surgeon to see both the location of the tumour and the extent to which it invades, our goal is to eliminate the risk that women require further surgery as the first operation did not remove all of the tumour,” says Clinical Research Fellow Dr Martha Kedrzycki, who is recruiting patients onto a trial that’s testing the system. “This technology could also be extrapolated for use in other cancers, aiding surgeons by highlighting targeted tissues.”