 Cardiovascular diseases (CVDs) have a significant impact on populations around the world. Affecting the heart and blood vessels, they are responsible for more deaths across the globe than any other cause.
Cardiovascular diseases (CVDs) have a significant impact on populations around the world. Affecting the heart and blood vessels, they are responsible for more deaths across the globe than any other cause.
Many people have surgery to treat their disease, so we rely on surgical methods to be effective and safe, both for clinicians and patients. Requiring high precision, these treatments are often guided by imaging techniques. Yet still, these methods are not foolproof. With heavy lead radiation aprons weighing down clinicians, and unclear imaging, there is much room for improvement.
Health systems are increasingly looking to robotics to answer difficult problems that humans cannot independently solve. Among some of our pioneering research taking place at our Hamlyn Centre, postdoctoral research associate Mohamed Abdelaziz has contributed to developing a robotic platform that can help improve the treatment of CVDs. The platform allows surgeons to offer precision in the operating theatre when making incisions, provide safer care to patients and reduce exposure to radiation from x-rays.
We caught up with Mohamed to find out more about the robotic platform.
What is the impact of CVDs worldwide?
CVDs include disorders such as coronary heart disease, deep vein thrombosis and pulmonary embolism. According to figures from the World Health Organization, there are 17.9 million deaths worldwide due to CVDs. So as the number one cause of mortality globally, it’s a big killer. Most deaths by CVDs are a result of heart attacks and strokes.
How are CVDs typically treated?
CVDs are mainly treated through a type of procedure called endovascular intervention. Here, clinicians carry out minimally invasive surgeries, cutting very small incisions and passing simple instruments through these incisions to the blood vessels. They treat the areas where there is clogging within the vessels, which cause strokes or other conditions.
Small incisions mean a quicker recovery for the patient. Traditionally patients used to have open surgery. They would be cut open, and surgeons would try to operate on patients from inside. This major surgery leads to a lengthy recovery.
What is the aim of your research?
I aim to develop a robotic system that assists surgeons to perform these surgeries. The procedures usually use imaging, so clinicians can see where their medical instruments are with respect to the patient’s body. Surgeons need the ability to see through the patient, which is why they use x-rays or fluoroscopy, which provides a continuous image in real-time.
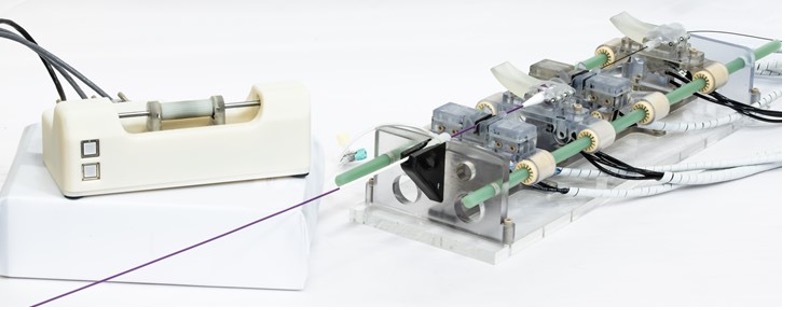
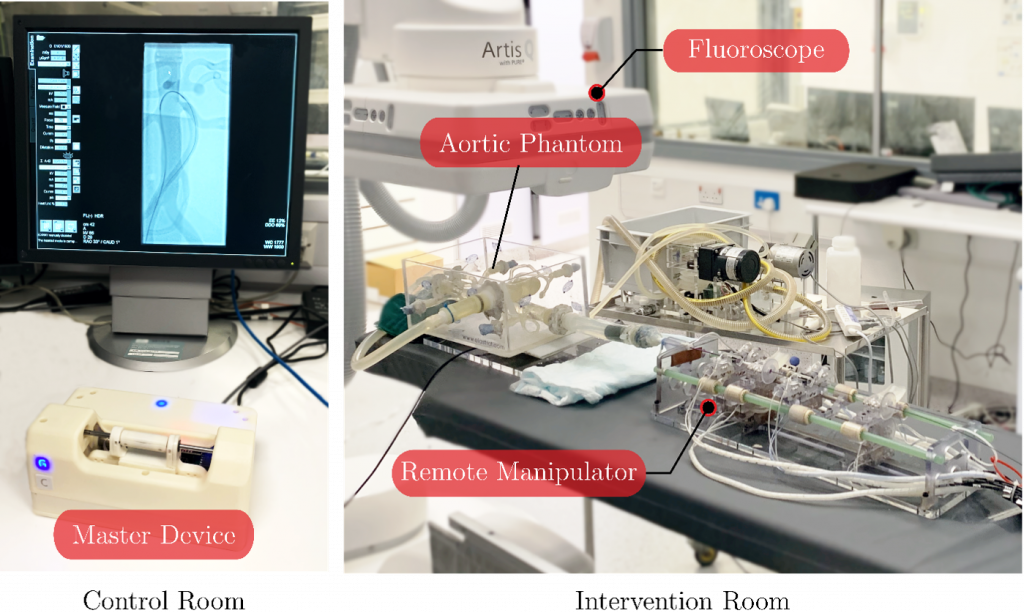
Over time, clinicians can suffer because of the exposure to high doses of radiation from the x-rays. This can affect their long-term health. Our idea to resolve this issue was to develop a “master-remote manipulator” robotic system. Here, the clinician is outside of the x-ray room, controlling the “master” device, while the “remote manipulator” inside the operating theatre mimics what the clinician does and carries out the surgery.
The clinician can then perform the procedure outside of the room, building, or even country.
How does your robotic platform work?
We wanted to develop a suitable system for different imaging techniques, including those that do not use radiation. One of these is magnetic resonance imaging or MRI. MRI has the unique ability to provide radiation-free imaging. Moreover, MRI can combine diagnosis, therapy, and early evaluation of therapy effectiveness in the same intervention.
Our robotic platform uses compressed air for manoeuvers, as this doesn’t affect the magnetic field that’s crucial for MRI or the imaging quality. At the same time, the entire robot is made out of plastic so it’s compatible with MRI. The remote manipulator is in the operating room and therefore does not get attracted to the magnet of the MRI.
What are the main benefits of using a robotic platform compared to traditional treatment methods?
Clinicians usually enter the x-ray environment wearing a heavy, bulky lead apron. You can imagine the load they have on their shoulders. The platform eliminates the need to wear the suit because they’re outside the room.
Our system also enables clinicians to receive haptic feedback, the sensation of touch, and through imaging we know where the surgical instruments are with respect to the blood vessels.
Clinicians usually insert these instruments and have inadequate feedback to determine whether these instruments have touched blood vessels or not. So, there is a risk of rupturing or damaging blood vessels if they apply too much force. The haptic feedback allows clinicians to feel a force opposing them to prevent these errors. The platform should therefore be much safer for the patient.
What stage are you currently at with your research?
We’ve concluded a user study and a pre-clinical animal study, where we assessed clinicians with different levels of expertise to perform the surgery both manually and robotically. These experiments were done while comparing different parameters, such as the time it takes to complete the tasks, the success rate of tasks and the forces posed by clinicians on the anatomy. Currently, we are planning to pursue further pre-clinical testing under MRI to benefit from its unique features.
What is your hope for the robotic platform?
I hope that it will be translational. I’d like clinicians to use it and patients to feel a difference. With medical equipment, it is not an easy process to go all the way from a functional prototype to a commercially approved product. Though the journey is lengthy, it’s an interesting one. You learn a lot – I’m an engineer, but I deal with clinicians and learn plenty from them.
Papers:
User study: An MR-Safe Endovascular Robotic Platform: Design, Control, and Ex-Vivo Evaluation
PhD Pitch Video: https://www.youtube.com/watch?v=P6quvBjopTI
Acknowledgements:
This research was funded by the UK Engineering and Physical Sciences Research Council, EPSRC, grant EP/N024877/1.