 Dr Alessandra Pinna is an Imperial College Research Fellow in the Department of Materials. Her research interests involve developing novel nanostructured ceramic and hybrid organic-inorganic coatings, nanoparticles and nanocomposites for biomedical applications, with a particular interest in drug delivery, antimicrobials and antioxidants. Dr Pinna was awarded the June Wilson Award 2021.
Dr Alessandra Pinna is an Imperial College Research Fellow in the Department of Materials. Her research interests involve developing novel nanostructured ceramic and hybrid organic-inorganic coatings, nanoparticles and nanocomposites for biomedical applications, with a particular interest in drug delivery, antimicrobials and antioxidants. Dr Pinna was awarded the June Wilson Award 2021.
Can you tell us more about your research area?
The key feature of my research is the use of inorganic materials and their dissolution ions as therapeutic agents, replacing the need for conventional drugs. In some cases, the inorganic ions (e.g. nanoparticles) can be more effective and more targeted than drugs, and cause fewer side effects.
What is the main aim of your research?
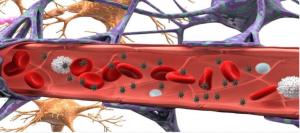
The main goal of my research is to develop an affordable, nanoparticle targeted drug delivery system that can penetrate across the blood-brain barrier (BBB) to treat different types of brain diseases such as Meningitis, Parkinson, and Alzheimer’s.
In collaboration with Francis Crick Institute, I’m currently researching the treatment of Tuberculous Meningitis (TBM) caused by a bacterium called mycobacterium tuberculosis, which is responsible for the most severe form of tuberculosis infection. I have used the sol-gel method to develop inorganic therapeutic nanoparticles. This is because it can produce nanoparticles at low temperatures with carefully controlled properties, using simple techniques. The nanocarrier is synthesised from biodegradable mesoporous silica nanoparticles (the vehicle), loaded with antibiotics (the drugs) and nanoceria (an anti-inflammatory agent), to kill the mycobacterium tuberculosis resident inside the brain and diminish the damage caused by inflammation associated with this infection.
Can you explain some of your recent results?
We have discovered that “spiky” nanoparticles can cross the blood-brain barrier in significant amounts and that silica mesoporous nanostars are better internalised by cells than spherical particles. Silica mesoporous nanostars, due to their high surface area, also demonstrated a higher loading capacity for antibiotics because of the spherical counterpart.
The novel multifunctional therapeutic nanostars that cross the blood-brain barrier and deliver the targeted drug to the brain could be a highly promising strategy to tackle any type of brain disease such as neurodegenerative disease, cancer or meningitis.
How could your results potentially benefit society?
Public Health England (PHE) is committed to meeting the World Health Organisation (WHO) Tuberculosis elimination targets by 2035. Reaching the WHOs End TB Strategy target by 2035 was always challenging, and the COVID-19 pandemic adds additional complexities.
Tuberculous Meningitis is the most severe form of tuberculosis infection. Worldwide, 100,000 individuals develop Tuberculous Meningitis each year, and 150 – 200 cases are reported in the UK. In general, those most at risk from Tuberculous Meningitis are children under four years, the elderly, and HIV-positive patients. Mortality rates can be high and in addition, around 30% of HIV-infected adults and 20% of children will suffer long-term after-effects from the infection.
The novel multifunctional therapeutic nanostars will enhance the delivery of antibiotics and anti-inflammatory by targeting the brain and achieving a controlled release of more than one drug at a time. Moreover, by providing new therapies for Tuberculous Meningitis, we will be able to tackle antimicrobial resistance.
What are your next steps are in your research? Are there any challenges ahead?
First, the big challenge is to prove the therapeutic efficacy of the nanostars. Once validated, their efficacy as a new therapeutic drug the translation strategy will be the next important step towards their use for other brain diseases.