
Currently, there are considerable gaps in the care of people with chronic obstructive pulmonary disease (COPD). Parris Williams, PhD student at the National Heart and Lung Institute (NHLI), highlights why improving the access, delivery and quality of annual COPD reviews is crucial to supporting 1.4 million patients in the UK with the condition.
Chronic obstructive pulmonary disease (COPD), a chronic condition causing restricted airflow and breathing problems, is the second most common lung disease in the UK. Currently 1.4 million people in the UK have a COPD diagnosis. Recommended by the British Thoracic Society and NICE guidelines, annual COPD reviews are a key element in COPD care. These reviews are an opportunity for the patient to discuss their condition with their medical team, alongside inhaler/medication revisions and opportunities for onward referrals if needed. When delivered correctly, COPD annual reviews increase the health and reduce exacerbation risk for patients.
Assessing the patient perspective
Using data from the Asthma+ Lung COPD patient passport, an online self-management tool that helps patients find out whether they’re receiving the care they’re entitled to, we discovered that, absence of an annual review was associated with significantly worse COPD care. This was particularly apparent among inhaler training, having a written care plan, and medication knowledge, following analysis of over 74,000 responses.
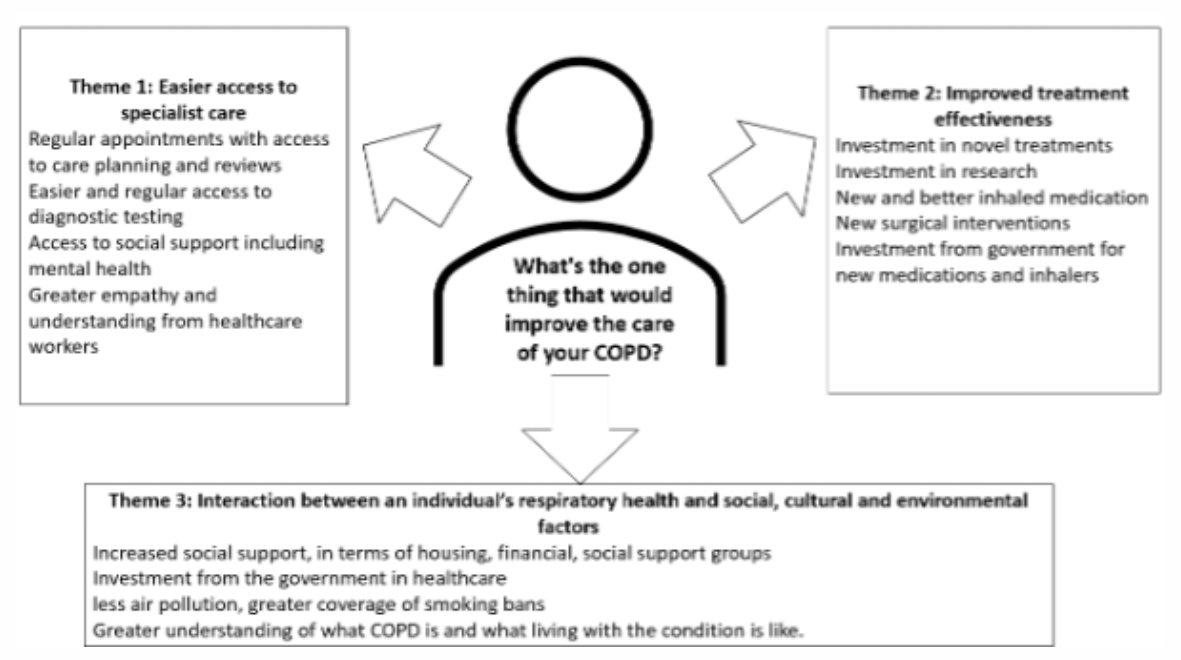
To assess the patient perspective, we also analysed over 4,000 responses from the 2020-2021 Asthma +Lung annual COPD survey, focusing particularly on the question “what’s the one thing that would improve your COPD care?” Three main themes were identified to improve patient care:
- Access and support from healthcare services
- Improved treatment effectiveness
- Interaction between COPD and the social environment.
This research highlights how the strain on the health service has negatively affected COPD care across the UK. This poor COPD care provision cannot be blamed entirely on the COVID-19 pandemic. The data used in the survey and previously published by the NHLI showed how COPD patients were missing out on fundamental aspects of their care before 2020. This current study highlights how this problem is getting worse.
A manifestation of ‘structural violence’
We have recently argued that COPD is a manifestation of ‘structural violence’ in our society – systemic factors that adversely affect people and cause injustice. In other words, something that has been done to individuals (e.g. growing up and living in poverty) as opposed to something that they have done to themselves (e.g. smoking). This current study therefore highlights how inadequate care is limiting patients experiencing the best possible health.
Despite the NHS’s long-term plan to increase provision and funding for respiratory diseases, our data highlights that care remains inadequate. Novel interventions such as GP-targeted education or utilisation of acute respiratory hubs may be successful interventions to increase the provision of COPD reviews.