Jenny Shelton highlights the potential for invasive and chronic fungal lung infections with Aspergillus fumigatus in COVID-19 patients and the dangers posed by growing antifungal resistance.
Virtually unknown just a few months ago, the COVID-19 pandemic has affected millions worldwide. The pathogen responsible, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), infects alveolar cells in the lungs. Parallels are already emerging between severe COVID-19 infection and severe influenza. Influenza, or ‘the flu’, is also caused by a virus that infects cells along the respiratory tract and is associated with similar symptoms to COVID-19 but has a lower death rate (<0.1%). Studies have found that up to 65% of individuals hospitalised with severe influenza infection are co-infected with bacteria. A recent review found 9 studies, undertaken in China and USA, that reported bacterial coinfection in a combined 62 of 806 (8%) individuals admitted to hospital with COVID-19 infection and the majority of patients (72%) received antimicrobial drugs.
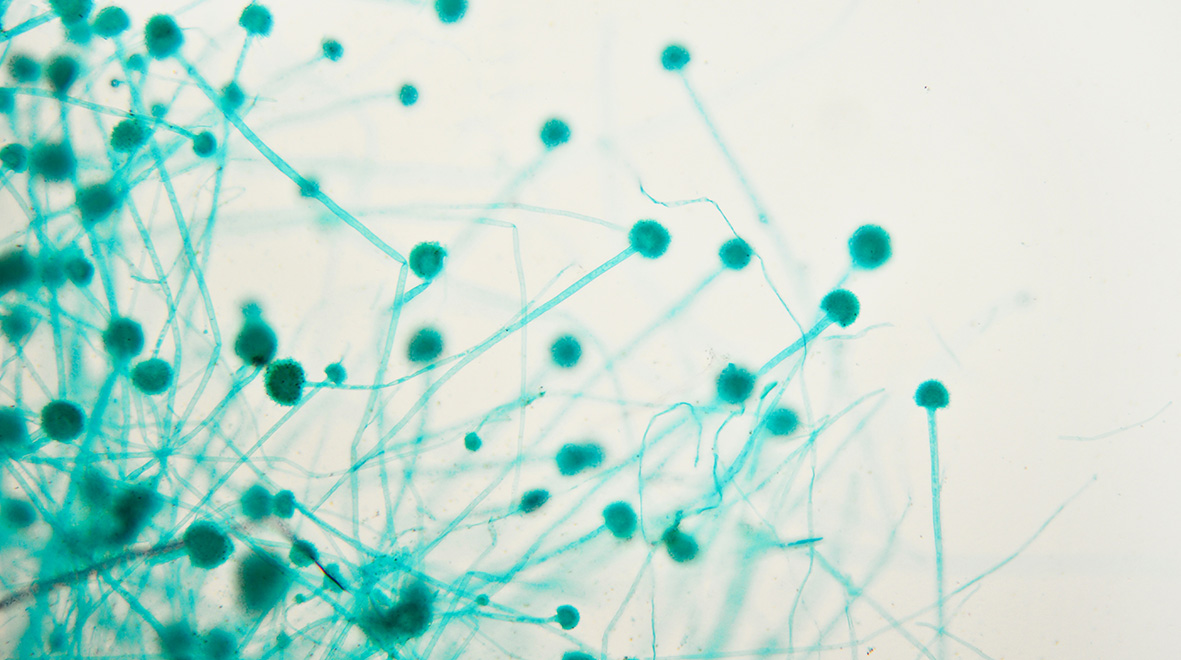
Another secondary infection associated with severe influenza is invasive pulmonary aspergillosis (IPA), which develops when spores from the fungus Aspergillus fumigatus grow in the lung and pass into the bloodstream to cause sepsis. IPA is diagnosed in up to 19% of individuals hospitalised with influenza, with significantly higher mortality in the patients with IPA. (more…)
