For World Leprosy Day 2018, Dr Tim Rawson explores how leprosy is not quite yet a disease of the past.
I have always found leprosy a fascinating disease. It is an incredible example of how microbiology, immunology, and social sciences can collide and impact significantly on human health.
Leprosy has been affecting humans for at least 4000 years. It has played a huge part in teaching us about disease caused by bacteria. In 1873 when Hansen discovered Mycobacterium leprae in tissue samples from patients with leprosy, this became the first bacteria to be directly linked to causing disease in humans. Since then we have developed an understanding of the complex range of types of leprosy that occur depending on how an individual’s immune system responds to the challenge of infection with Mycobacterium leprae. We have also observed the consequences of the deformities and disability caused by the body responding to Mycobacterium leprae, which favours human nerves and skin. In turn, we have seen how the appearance of individuals with disability and disfigurement from leprosy has driven stigma, misinformation, and the discrimination of those affected by the disease.
For many people in the UK and around the world, leprosy, or Hansen’s disease, is an ancient condition of our ancestors. It is something that we hear about in religious scripture or watching films like Ben-Hur or the Life of Brian. Associated with exile from communities, deformity, and poverty. Something that no longer affects the modern world that we now live in.
Leprosy is often referred to in Sanskrit from around 1400 BC, with the term “kushtha” used to describe it. This translates to “eating away”. Courtesy of Wellcome Collection.
In 2000, the World Health Organisation (WHO) made an announcement that leprosy had been eliminated as a public health issue, with the global prevalence finally falling below one case per 10,000 people. This was the culmination of many years of identifying and treating patients with leprosy. This included the development of multi-drug therapy – a real game-changer in the treatment of Hansen’s disease. In total, over 16 million people affected by leprosy were treated, often free of charge. This was a great success.
And so for the elephant in the room. If we have eliminated leprosy as a public health problem, why do we still need to worry about World Leprosy Day?
There is still work to be done
Well firstly, the target for elimination of leprosy (less than 1 in 10,000 prevalence) was selected on the observation that at this point a disease would often seem to disappear from a community. However, it soon became clear that the potential for disease transmission may still remain. And this got the epidemiologists worried.
In fact, it was something called the New Case Detection Rate (NCDR) – a proxy for the incidence of a disease – that seemed to be a more accurate indicator of the potential for ongoing disease transmission within a community. And when the experts looked at the NCDR, this had, overall, remained pretty static despite the significant impact multi-drug therapy had in reducing the prevalence of leprosy globally. There are still a number of unknowns in terms of transmission of leprosy and how to interrupt it (that would lead to the true eradication of leprosy).
Admittedly, whilst leprosy does not have a large impact on our communities in the UK anymore (although you may be surprised that between 2003 and 2012 there were 139 cases in the UK reported to Public Health England) there are still around 210,000 new cases diagnosed worldwide every year. Leprosy still affects people in over 100 countries and remains one of the leading causes of long-term nerve damage, called neuropathy, worldwide.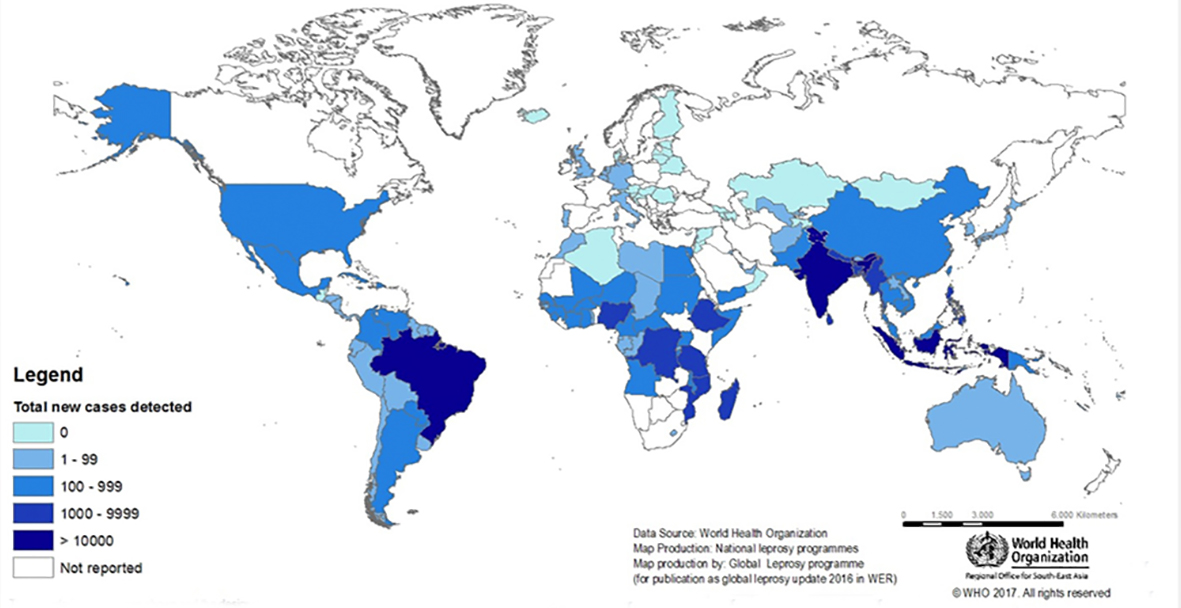
Geographical distribution of new leprosy cases, 2016. Courtesy of WHO.
When considering how to interrupt the transmission of leprosy an interesting observation can be made about the interaction of leprosy with other Mycobacterial infections, such as tuberculosis. For example, the BCG vaccination with Mycobacteria bovis, commonly used for protection against tuberculosis, has also been demonstrated to protect against the development of leprosy. In fact, in many cases it actually appears to be more protective for leprosy than tuberculosis. Furthermore, it is likely that the co-existence of leprosy and tuberculosis within communities helped to drive the elimination of leprosy from Europe long before we had effective medical treatments. This may have been due to the immune response in someone with leprosy predisposing them to more severe concomitant infections with tuberculosis.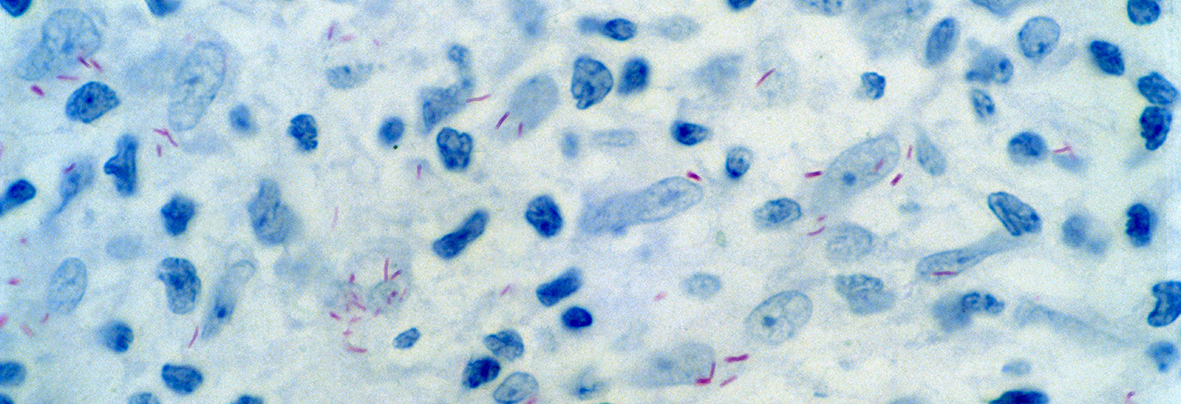
Mycobacterium leprae in the skin from a patient diagnosed with leprosy. The bacteria stain red. Courtesy of Wellcome Collection.
Raising awareness of an age-old disease
A further area for consideration is raising awareness of the condition and integrating leprosy services within mainstream healthcare. I have deliberately not delved into the stigma and cultural challenges that must be addressed in dealing with leprosy here, but I do want to touch on awareness and training of healthcare professionals. This is especially important in endemic regions, which often have high rates of other neglected tropical diseases and non-communicable diseases, like diabetes. These conditions can often present with overlapping symptoms and even together. Reports of doctors missing early opportunities to diagnose leprosy are increasing, particularly in India where diabetes (a leading cause of nerve damage) is estimated to affect over 80 million people by 2030. Therefore, training of healthcare professionals remains a key priority to ensure that diagnosis is not delayed, which will often lead to further disability if treatment is not commenced promptly and the disease is allowed to progress.
There is also a focus on the integration of leprosy services into other areas of healthcare to ensure that skills are maintained and to reduce the perception of the disease as peripheral and something that has to be kept away from other medical problems. This should help to reduce some of the stigma that continues to shroud leprosy.
Progress towards a leprosy-free world
So despite the elimination of leprosy being announced in 2000 by the WHO; this wasn’t the end of leprosy. It has continued to cause disease and disability in hundreds of thousands of men, women, and children on a yearly basis. Stigma and misinformation about the disease have continued to be barriers to early detection and treatment. This is despite the fantastic steps made by many non-governmental organisations who work tirelessly to address these problems, including Lepra, who I have been fortunate enough to be supported by previously.
In 2016 the WHO published their new strategy for 2016-2020: Accelerating towards a leprosy-free world. This strategy aims to promote early detection of leprosy before the presentation of visible disability whilst improving health coverage and access for marginalised populations. A major aspect of this is increasing awareness and reducing the stigma that surrounds leprosy.
And so on this World Leprosy Day, spend a moment to consider this very ancient disease that still has a huge impact on the lives of hundreds of thousands of people every year.
Dr Timothy Rawson (@TmRawson) is a junior doctor and currently undertaking a PhD with the NIHR Health Protection Research Unit in Healthcare Associated Infections and Antimicrobial Resistance at Imperial’s Department of Medicine.
Lead image courtesy of Wellcome Collection CC BY 4.0: Leprosy: a patient uncured and a patient cured, the latter pointing to an allegory of early treatment. Colour lithograph.
Following the launch of the Faculty of Medicine’s reorganised academic structure on 1 August 2019, this post was recategorised to Department of Infectious Disease.
Hi. Am writing on leprosy after a significant Supreme Court judgment in India on how leprosy patients need to be given a better deal. Grateful if I could interact with Dr. Rawson on email and possibly quote him.
I am the contributing editor of a weekly magazine called India Legal.
Hi Ramesh. You can find Dr Rawson’s email in his profile: http://www.imperial.ac.uk/people/timothy.rawson07
Thanks
Can you identify the demographic that’s spreading all the disinformation?
Orissa, a state in India, has recorded 9,576 leprosy cases in 2018-19 which is down by 469 cases from the previous year. Awareness activities from govt helped to reduced these numbers.
Today, over four million people live with leprosy-related disabilities, and it remains one of the leading causes of long-term nerve damage worldwide.
Thansk Mr. Rawson to share your part of research on Leprosy.
You’ve shared WHO published their new strategy for early detection, so is that by any test like T.B or is it by using any Machine.
Kindly Share your knowledge on this.
I am really impressed with your blog article, such great & useful knowledge you mentioned here. Your post is very informative.
Such a great post.
It’s really a very informative post about the Leprosy which becomes a public health problem today.
Thanks for this informative article about Leprosy which becomes a public health problem today.
Thanks For sharing this Wonderful Content
Great post
Thanks for sharing this informative post about leprosy such great and informative knowledge share thank u
Hello Admin,
Thank you for sharing this piece of info. And, it reminds of my clinical posting in one of the leprosy unit way back 2000. It’s been 20 years , i still doubt it is not completely eradicated despite effective regimen and strong implications from respective health boards around the world.
Very well written
very useful post
thanks for sharing
Today, over four million people live with leprosy-related disabilities, and it remains one of the leading causes of long-term nerve damage worldwide.