On Mesothelioma Awareness Day, Dr Anca Nastase provides an insight into mesothelioma and how research advances offer new hope for improved treatment.
Mesothelioma Awareness Day represents a great opportunity to gain more information about the disease biology, risk factors or symptoms from everyone in the mesothelioma community. Raising awareness is essential as it has the potential to improve prevention and early diagnosis and can translate into better outcomes and better survival for the patients.
My aim as a scientist within the National Centre for Mesothelioma Research (NCMR) is to deepen the molecular research in mesothelioma and to advance our understanding of the mechanisms responsible for the onset and progression of this disease.
Although progress has been made in the field, further understanding of the pathophysiology is still desperately needed.
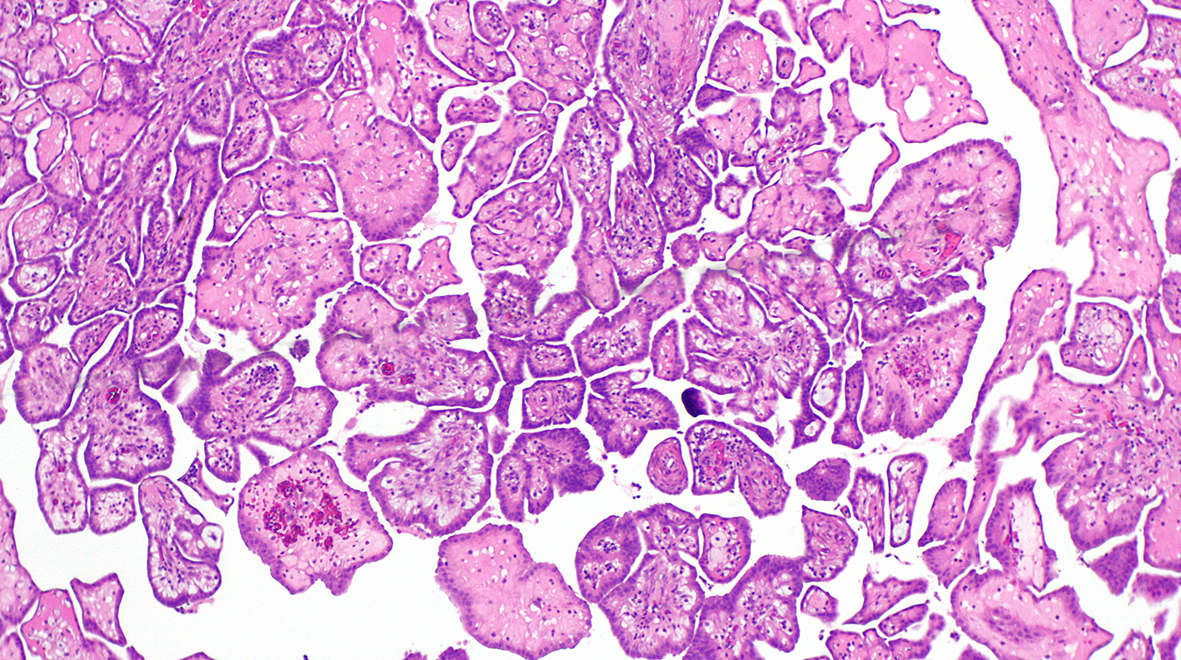
Mesothelioma is a type of cancer that arises and develops in the thin layer that covers the human internal organs, called mesothelium.
Based on the organ of onset, mesothelioma is classified into: pleural, developing in the lining of the lungs; peritoneal, in the abdominal cavity; and pericardial, in the heart sac and testicular, in the testis. About 80% of all mesothelioma cases are pleural mesotheliomas, with male individuals having a higher incidence and mortality. The disease is more commonly diagnosed at an older age. Symptoms sometimes overlap with those of other diseases and could challenge and delay the correct diagnostic and therapeutic intervention.
Asbestos exposure
The majority of mesothelioma cases develop after a person is exposed to and inhales asbestos fibres for a long time. The strong connection between asbestos exposure and mesothelioma has been shown for more than half a century, making asbestos the main risk factor for the disease.
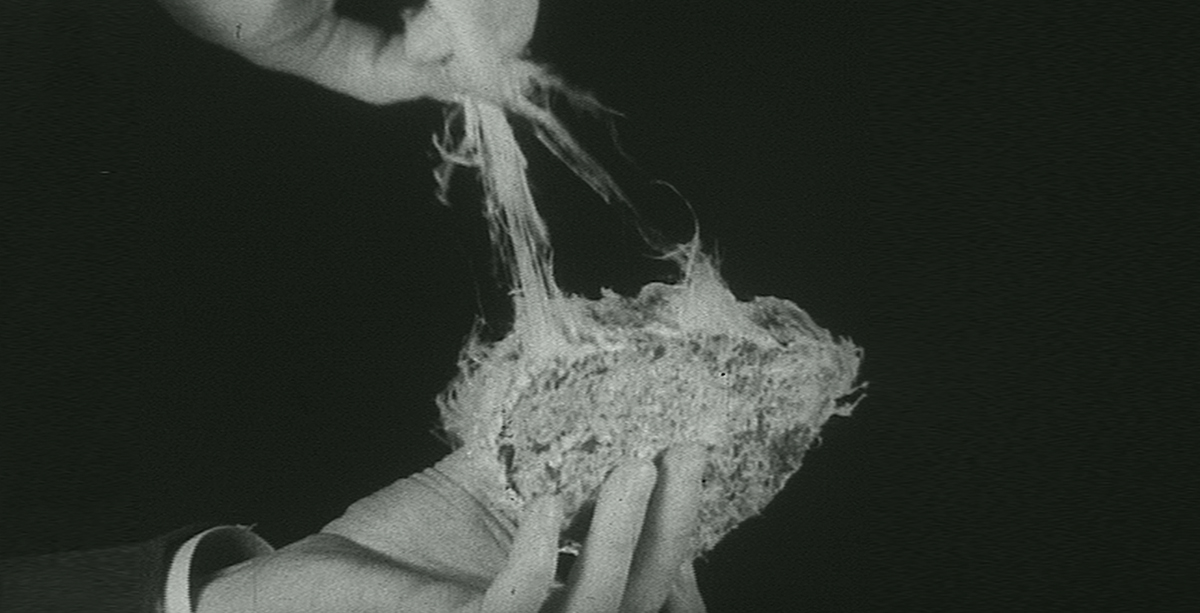
Asbestos is a group of six naturally occurring silicate minerals made up of thin fibres which were commonly used in the past as a building material due to its properties. Based on the fibre appearance it divides into two groups: serpentine, with long and curly fibres and amphibole, with short, needle-like fibres. All asbestos is considered harmful and classified as type I carcinogen, if disturbed, with the amphibole group and specifically the amosite (brown asbestos) and crocidolite (blue asbestos) within this group being most hazardous.
In the UK a ban on the import and use of blue and brown asbestos was imposed in 1985, followed by a ban on chrysotile (white asbestos) from the serpentine family in 1999. There is a lag of 20-50 years between exposure to asbestos and onset of the disease, and so despite the prohibitions in place, in the UK the estimates are that the number of cases will peak between 2020 and 2025.
Though mesothelioma is an aggressive cancer, with less than 10% of the patients surviving at 5 years, due to late diagnosis, it is considered a rare type of cancer. According to Cancer Research UK, there are 2700 new mesothelioma cases every year in the UK compared to 47000 new lung cancer cases or 55000 new invasive breast cancer cases. Unfortunately, often these statistics translate into low funding for this deadly disease compared to other cancers.
Promising therapies
From the beginning of our research at NCMR and based on previous data available, it was clear that mesothelioma is characterized by a few genomic alterations, unlike lung cancer or melanoma which both have a recognized carcinogen as a risk factor, just like mesothelioma. This genomic landscape usually translates into a paucity of therapies available and no effective targeted therapies. For example, there are over 5000 clinical trials for lung cancer either recruiting or completed listed on clinicatarils.gov compared to merely 300 for mesothelioma. Very recently, a ray of hope came in the field of therapy with the addition of immune checkpoint inhibitors, nivolumab plus ipilimumab, for the first-line treatment of adult patients with unresectable pleural mesothelioma.
Through our fundamental research, we have identified genomic vulnerabilities that can potentially be targeted by known therapeutics and we have refined our understating on the mechanisms that are operating within tumours. I believe that fundamental research is essential for providing novel insights on the intrinsic causes of mesothelioma and could help develop better strategies to limit the number of cases and improve survival.
However, mesothelioma, just like other cancers, is a dynamic disease, characterized by heterogeneity and genomic evolution. We recognize today the importance of not only deciphering the genomic aberrations that are present within a tumour but also understanding the role that the tumour microenvironment and the immune system have in tumour evolution and in developing tumour resistance to therapies.
Continued systemic research and progression towards precision medicine are imperative in mesothelioma. Every new piece of information that we gain at the bench side end has the potential to affect the healthcare system and the patients.
It is the path from fundamental science to translational medicine and clinical work together with multi-disciplinary teams collaboration that will ultimately translate into early diagnosis, state-of-the-art treatment options and, most importantly, prevention to decrease the incidence of mesothelioma.
Dr Anca Nastase is a Postdoctoral Research Associate at the National Centre for Mesothelioma Research based at Imperial’s National Heart and Lung Institute.
Header image: Wikimedia Commons