
Ellen Grimas draws on her PhD research investigating the role of coparenting in children’s development and behaviour.
I remember a child psychiatrist saying during a keynote at a conference that the only mental health that mattered was child mental health. This made me think back to working at a mental health crisis house, where I was often struck by how many people said their symptoms first emerged in childhood or adolescence. Research tells a similar story, with recent figures suggesting that 75% of mental health problems emerge before the age of 18, and yet only 30% of people reported receiving proper and timely support.
This is worrying as there is a wealth of research suggesting that early intervention is not only beneficial for the individual and their family, but also for society as a whole. Childhood is clearly a key period in the development of our mental health, and also offers a unique opportunity to intervene. So, although it may not be the only mental health that matters, it is evidently an incredibly important component. In the context of an over-stretched NHS, the idea of low-level interventions in childhood that could help avoid the need for services in later life is a powerful one.
Moving from cure towards prevention
This idea underpins much of my work as a PhD candidate and research assistant working on an early intervention trial lead by Professor Paul Ramchandani at the Centre for Psychiatry. The Healthy Start, Happy Start study is testing the effectiveness (both in terms of cost and patient outcomes) of an early intervention programme called VIPP-SD. This aims to support parents of young children at risk of behaviour problems, such as aggression, tantrums and poor attention. Although these issues in childhood are often transient, for a significant proportion of children they persist, affecting them throughout their lives. This includes a greater risk of mental health problems, physical health problems, and social outcomes such as school attainment and alcohol problems.
The importance of mothers and fathers in child mental health
The programme we are testing uses something called video-feedback, where short clips are taken of parents doing everyday things like playing together, reading or sharing a meal. Parents then review the clips with a trained professional who provides positive feedback on areas where parents are already doing well, as well as offering tips for managing more challenging moments. The intervention has been shown to be effective at improving parent behaviour. There is also some evidence suggesting benefits for children, including improvements in behaviour and social and emotional outcomes. This research has been conducted in other countries and settings, but Healthy Start, Happy Start is the first study to test video-feedback in a real world NHS context, with NHS services and UK families.
One thing that makes the Happy Start study unique is that both mothers and fathers are invited to take part. Looking at the literature into parenting programmes, it’s clear that fathers are very rarely invited to participate. Indeed, some fathers report that the word ‘parent’ has practically lost meaning to them, as they thought it had become synonymous with the word ‘mother’. This pattern of overlooking fathers from parenting research and services is frustrating, as we know fathers play a hugely important role in children’s development. We also know that parenting programmes are more effective when they participate. In the Happy Start study, we invited fathers to take part either on their own or with their partner and received a really positive response. The data from families where both parents take part forms the basis of my thesis.
The importance of good coparenting
I am interested in seeing whether the programme (VIPP-SD) might lead to improvements in the way that parents coordinate care and cooperate when interacting with their child. We know that this behaviour, called coparenting, is another good predictor of child outcomes in the long- and short-term. All coparents – regardless of whether they are divorced, living apart, or in a cohabiting relationship – may sometimes find it challenging to work together and share the enjoyment of everyday moments with their child. Coparenting captures both the negative and positive aspects of this relationship: from contradicting each other and arguing in front of the child, to positive factors, like having fun together and working well as a team. I’m interested in seeing whether this programme might support families in becoming more cooperative coparents and whether these benefits are passed on to their child, and more specifically whether it ultimately improves mental health outcomes. This research would further the argument that fathers should be routinely invited to participate in their child’s health care, and that parents play a key role in their child’s development in many different ways. It may also strengthen the argument for early intervention being made more widely accessible.
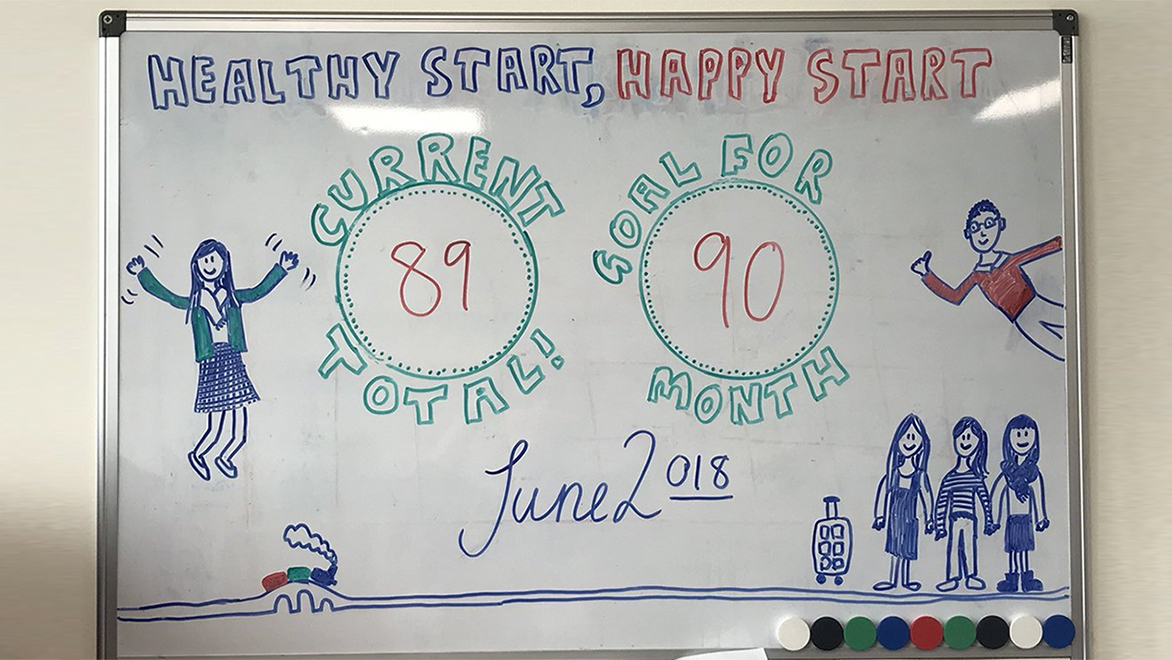
2019 is a big year for the Happy Start study
After four years of research visits with families, we are due to finish data collection this May. We are excited to see whether the programme is helpful, and whether it could be something routinely offered to families who are part of early years’ services. As well as answering this main question, I am one of a team of other PhD students, academics, researchers, trainee child psychiatrists and clinical psychologists who are all using data from the study to answer other important questions about early child development and mental health. These questions range from seeing whether the programme is differentially helpful to children depending on their genes, to the validity and reliability of new assessment measures for use with young children. We hope these studies will add to the growing literature about the value of early intervention, and the importance of supporting child mental health.
Ellen Grimas (@EllenGrimas) is final year PhD student in Clinical Medicine for Research at the Department of Medicine and is supervised by Professor Paul Ramchandani and Dr Christine O’Farrelly.
Healthy Start, Happy Start is funded by the National Institute for Health Research (NIHR) Health Technology Assessment Programme.
Following the launch of the Faculty of Medicine’s reorganised academic structure on 1 August 2019, this post was recategorised to Department of Brain Sciences.