In low- and middle-income countries (LMICs), a notable number of individuals have smaller lungs for their sex, age, and height, especially in South and East Asia, as well as sub-Saharan Africa. The key question: Why does this pattern persist in these regions?
This phenomenon extends beyond physiological concerns, and as indicated by recent studies, reveals a troubling link between smaller lungs and heightened risks of suffering from heart disease and diabetes. Dr André Amaral, an epidemiologist at the National Heart and Lung Institute (NHLI), explores this phenomenon.
The BOLD study
Chronic lung diseases affect millions of people of all ages worldwide. Approximately 20 years ago, the Burden of Obstructive Lung Disease (BOLD) study was set up by Imperial College London to find out more about the prevalence and determinants of chronic obstructive pulmonary disease (COPD), which back then, was already considered a leading cause of disability and death.
The BOLD study was conducted in 41 sites across Africa, Asia, Australia, Europe, the Caribbean and North America, and recruited more than 30,000 adults aged 40 years and over. The large coverage of world regions, and ethnic groups, as well as the large number of participants, all answering the same questions and undergoing the same measurements in a standardised manner, makes the BOLD study unique. Participants in this study provided information on several characteristics of their life. This included whether they had been diagnosed with lung disease, a heart disease, or diabetes, whether they smoke or ever smoked, their weight and height, and their highest level of education. The level of their lung function was measured through a medical test called spirometry, which measures how much air a person can breathe out in one forced breath.
(more…)
Read Unravelling the mystery of smaller lungs in low- and middle-income countries in full

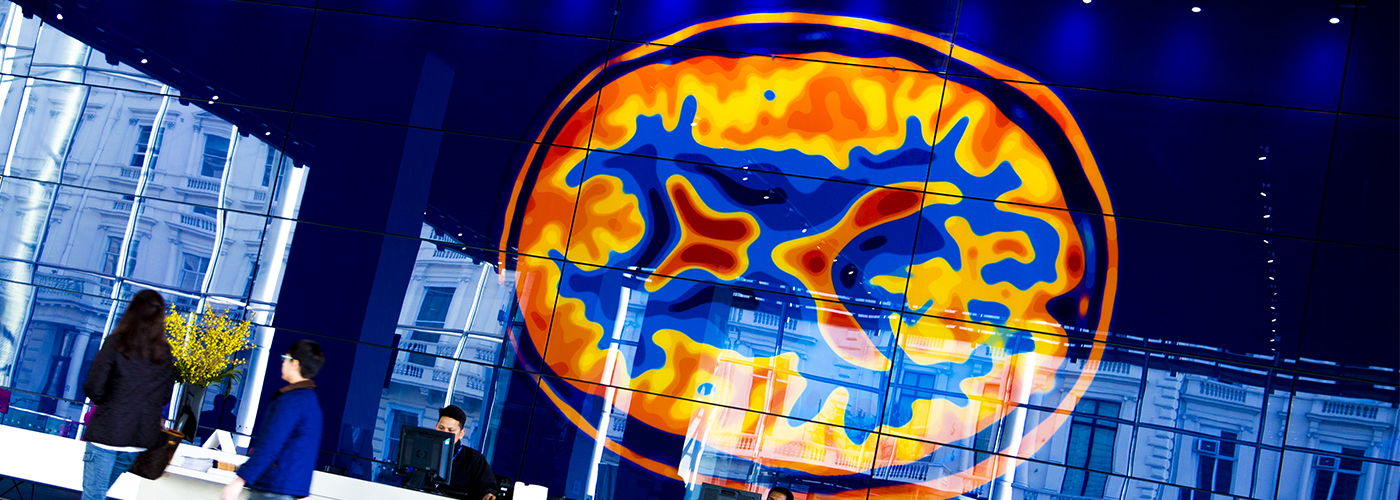
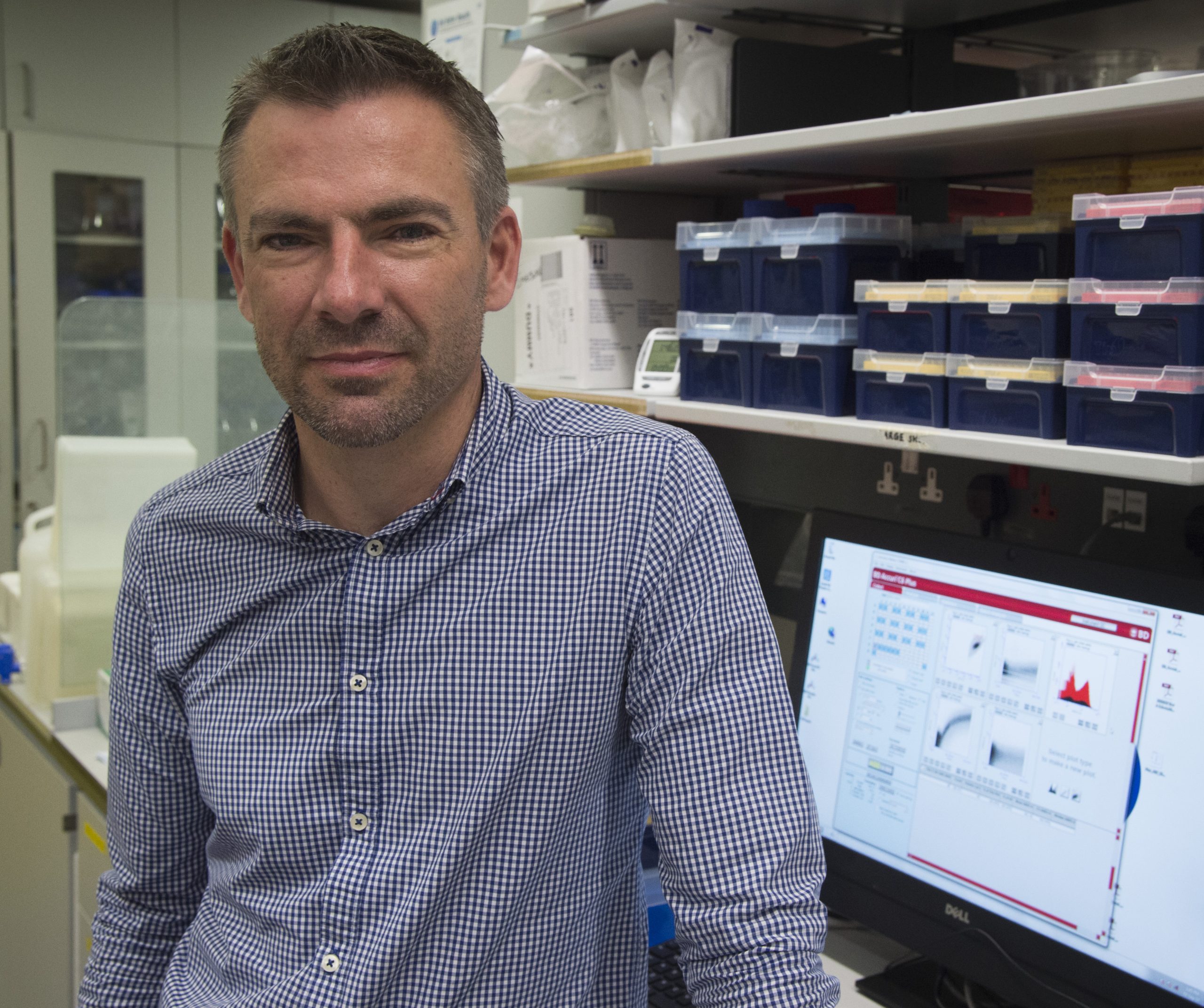 Born on what would eventually be recognized as World AIDS Day in the 1970s, Dr Mike Emerson, now affiliated with the National Heart and Lung Institute, relocated to vibrant London during the early 1990s amidst the fervour of the Britpop era. In the backdrop of Blur and Pulp melodies, 1990s London faced the AIDS crisis. Three decades later, he is at the helm of a team investigating cardiovascular ailments in people with HIV. In this piece, Dr Emerson reflects on the advancements in HIV diagnosis and therapy, and reiterates the ongoing importance of National HIV Testing Week.
Born on what would eventually be recognized as World AIDS Day in the 1970s, Dr Mike Emerson, now affiliated with the National Heart and Lung Institute, relocated to vibrant London during the early 1990s amidst the fervour of the Britpop era. In the backdrop of Blur and Pulp melodies, 1990s London faced the AIDS crisis. Three decades later, he is at the helm of a team investigating cardiovascular ailments in people with HIV. In this piece, Dr Emerson reflects on the advancements in HIV diagnosis and therapy, and reiterates the ongoing importance of National HIV Testing Week.