
This month, people worldwide will take on the 31-day ‘Sober October’ challenge, a movement that began in the UK to raise funds for Macmillan Cancer Support, benefiting those with cancer. Even if you’re not officially participating, Sober October offers a chance to reset your body and rethink your relationship with alcohol. In our latest blog, Professor David Nutt from the Department of Brain Sciences shares expert tips on how to make the most of this healthy, alcohol-free month.
Sober October is here, and it’s the perfect opportunity to hit reset on your relationship with alcohol – whether you’re looking to completely abstain or simply cut down. Much like Dry January or Dry July, this month-long challenge is about taking a break from alcohol and reassessing its place in your life.
With alcohol consumption on the decline among Gen Z and Millennials, it’s clear that more and more people are recognising the benefits of taking a break from booze and now is the perfect time to jump on board.
Sober October is a global movement encouraging people to stop drinking for the month of October. For many, it’s a time to take a break and rest after summer’s social gatherings and prepare for the end of year holiday season with a clearer mind. It’s not just about abstinence; it’s also about fostering better health, improving mental clarity, and building positive habits for the future.
Progress not perfection
Stopping alcohol intake for a whole month can have major health benefits. People who participated in previous abstinence challenges like Dry January have reported improved sleep (56%), weight loss (38%), and better mental health. Even those who didn’t make it through the full month still saw long-term reductions in alcohol intake and enhanced well-being, showing that it’s about progress, not perfection. There are also likely to be measurable physiological improvements such as lowering your blood pressure if you are hypertensive, losing weight (as alcohol has more calories than most people imagine) and putting more money in your pocket – perfect for upcoming holiday shopping.

 The path to a smokefree generation demands decisive action and innovative strategies. To mark World No Tobacco Day,
The path to a smokefree generation demands decisive action and innovative strategies. To mark World No Tobacco Day, 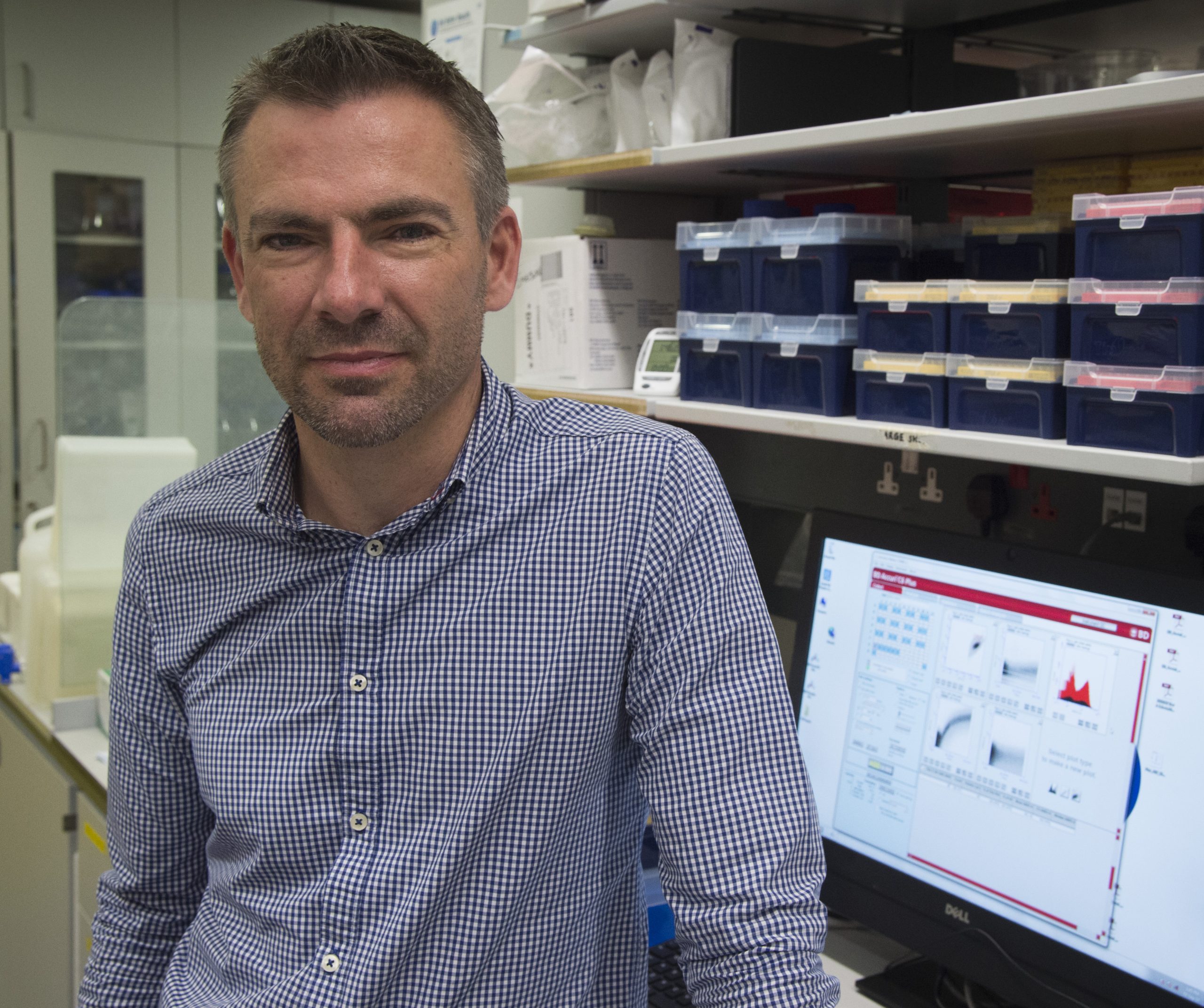 Born on what would eventually be recognized as World AIDS Day in the 1970s, Dr Mike Emerson, now affiliated with the National Heart and Lung Institute, relocated to vibrant London during the early 1990s amidst the fervour of the Britpop era. In the backdrop of Blur and Pulp melodies, 1990s London faced the AIDS crisis. Three decades later, he is at the helm of a team investigating cardiovascular ailments in people with HIV. In this piece, Dr Emerson reflects on the advancements in HIV diagnosis and therapy, and reiterates the ongoing importance of National HIV Testing Week.
Born on what would eventually be recognized as World AIDS Day in the 1970s, Dr Mike Emerson, now affiliated with the National Heart and Lung Institute, relocated to vibrant London during the early 1990s amidst the fervour of the Britpop era. In the backdrop of Blur and Pulp melodies, 1990s London faced the AIDS crisis. Three decades later, he is at the helm of a team investigating cardiovascular ailments in people with HIV. In this piece, Dr Emerson reflects on the advancements in HIV diagnosis and therapy, and reiterates the ongoing importance of National HIV Testing Week. 




