
This festive period, Three Wise Women from the Faculty of Medicine will be giving us the gift of wisdom.
Dr Rasha Al-Lamee, Clinical Reader in the National Heart & Lung Institute and Clinical Academic Interventional Cardiology Consultant at Imperial College Healthcare NHS Trust, highlights the unique strengths of the UK’s life sciences research ecosystem, from the NHS to the invaluable contributions of patients. She reflects on her groundbreaking ORBITA trials, which challenged conventional wisdom about stenting for coronary artery disease. Dr Al-Lamee also shares how these experiences have shaped her career and passion for mentoring the next generation of cardiologists.
We are fortunate in the UK to have a well-developed infrastructure for research in life sciences. Our universal healthcare system within the NHS, world-leading academic institutions, and dedicated researchers provide a unique environment for innovation. Most importantly, it is our incredible patients—who not only understand the need for research but are willing to participate—that make groundbreaking studies possible. This unique combination allows us to lead the world in delivering research that tests novel treatments, evaluates existing practices, and paves the way for guideline-changing clinical practice.
As a clinical trialist, I have been privileged to work within this exceptional ecosystem. It has allowed me to carry out work that I do not believe could have been conducted in many other places in the world. My focus has been on treatments for ‘stable’ coronary artery disease, a condition that affects around 2.3 million people in the UK and causes chest pain, breathlessness, and sometimes pain throughout the body. Treatments often include medicines or angioplasty, a procedure where stents—wire mesh tubes—are placed into arteries to open blockages. However, since its introduction, there has been ongoing debate about whether the relief patients experience is due to the procedure itself or a placebo effect.
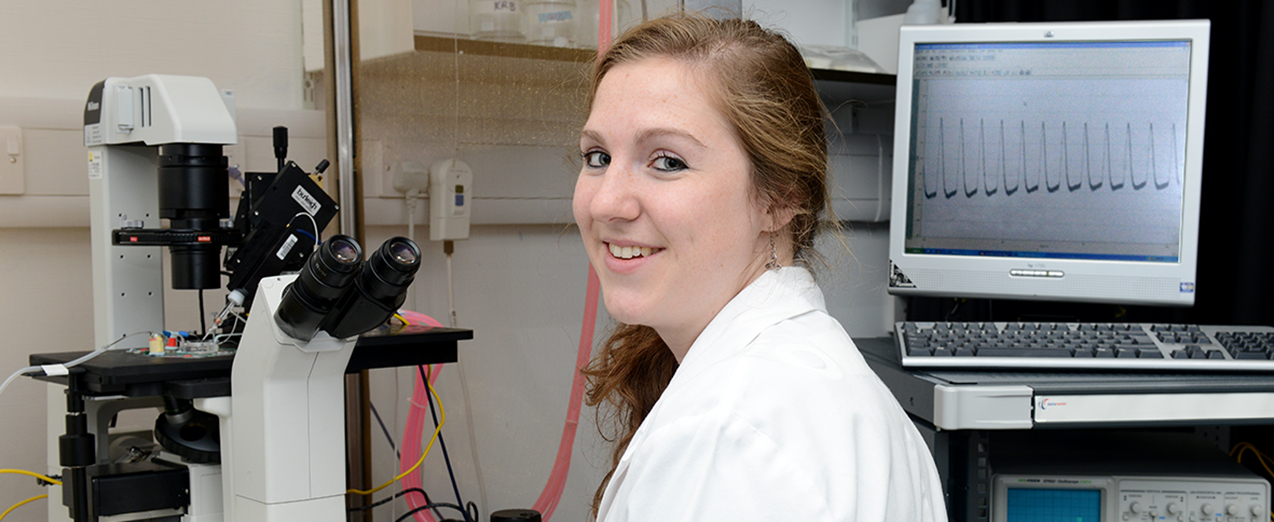
 Many researchers study a particular disease because they have a personal connection to someone who has been affected. For researcher Dr Nicky Whiffin, it happened in reverse.
Many researchers study a particular disease because they have a personal connection to someone who has been affected. For researcher Dr Nicky Whiffin, it happened in reverse.




 Dr Amit Kaura,
Dr Amit Kaura,