Dr Emma Smith—HIC-Vac Network Manager—explains how specific guidelines for the provenance and manufacture of challenge agents could make human infection studies even safer.
Human infection studies, also known as human challenge studies, are clinical trials where volunteers are intentionally given a carefully considered dose of a pathogen—known as the challenge agent. These models can be used to study host-pathogen interactions and disease progression; identify and test the efficacy of promising vaccines and drugs in development; or be used as proof-of-concept studies for testing novel medications. In this controlled environment it is possible to study infections in ways that aren’t possible in traditional field studies.
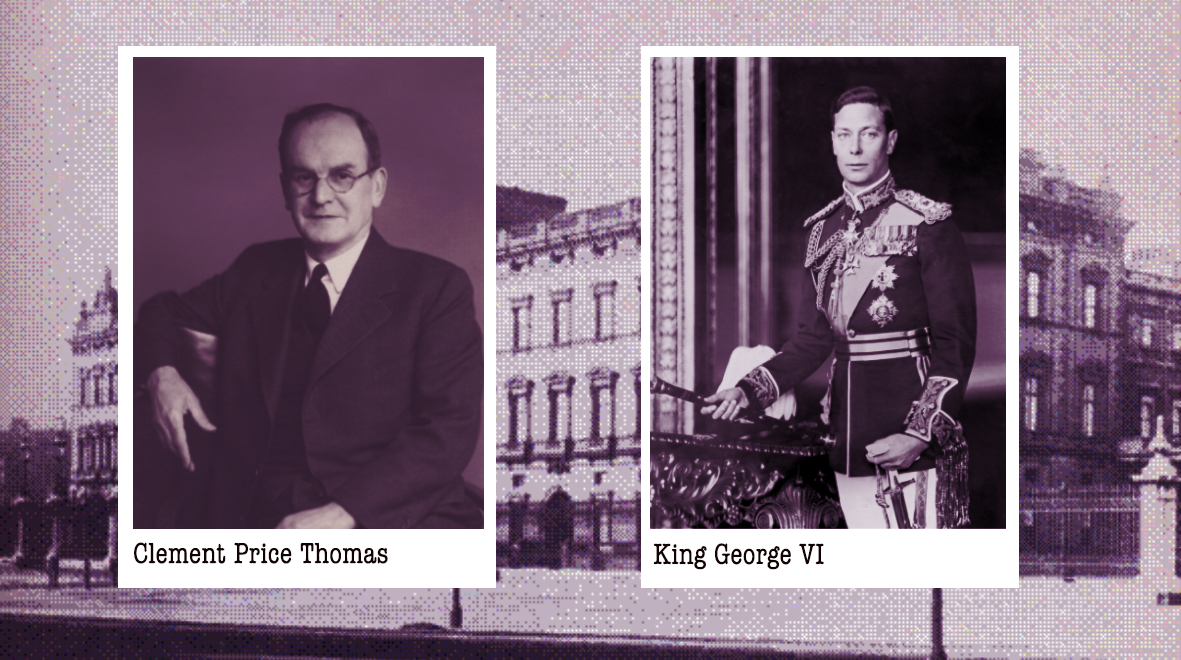
One of the first steps towards establishing a challenge study is the selection, isolation, development and production of the challenge agent. However, unlike medicines, the regulation of challenge agent manufacture varies internationally; an area that the research community has identified as a potential weakness in the field. Although human challenge studies have an excellent safety record—a recent literature review identified just 24 Serious Adverse Events (SAE) and zero deaths or cases of permanent damage among 15,046 participants in 308 studies spanning 1980 to 2021— the lack of specific guidelines for the provenance and manufacture of challenge agents warrants attention.
HIC-Vac—an Imperial-led international network of researchers who are developing human infection challenge studies—has been working with the global charitable foundation Wellcome and the company hVIVO to address this unmet need. Our purpose was to promote volunteer safety whilst maximizing access to challenge agents and challenge models globally. (more…)